Characterizing the Distinct Glycemic Patterns Of Post bariatric Hypoglycemia (PBH)
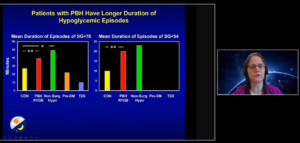
DANIEL LEE, et al conducted a study to characterize the distinct patterns of post bariatric hypoglycemia which was presented at the virtual ADA 2020 session. The authors used blinded CGM (Dexcom G4) to characterize glycemia, glycemic variability (GV), and severity and length of hypoglycemia in patients with PBH with prior roux-en-Y gastric bypass (PBH, n=40). The authors compared results to those of individuals with reactive hypoglycemia with no prior GI surgery (Hypo, no-GS, n=20) and to publicly available Dexcom G4 data from 3 additional groups: healthy controls (HC, n=38), prediabetes (Pre-DM, n=14), and T2D (n=5). Metrics assessment was carried over 24 hours as well as during daytime (6 AM to midnight) and nighttime (midnight to 6 AM) independently. Mean and median sensor glucose (SG) were similar for PBH and HC (mean: 99.8±18.6 vs. 96.9±10.2 mg/dL; median: 93.0±14.8 vs. 94.5±7.4 mg/dL, p>0.05 for both). By contrast, PBH had higher coefficient of variation (27.3±6.8 vs. 17.9±2.4%, p<0.0001) and a wider range and IQR of SG values (range: 154.5±50.4 vs. 112.0±26.7 mg/dL; IQR: 28.0±7.4 vs. 20.0±4.4, p<0.0001 for both). Nadir SG was lowest in PBH (42.5± 3.7 mg/dL vs. other groups, p<0.0001) with statistical significance vs. HC (49.0±11.9 mg/dL, p=0.0046). PBH had greater percentage of time with SG<70 mg/dL vs. HC (7.7±8.4 vs. 3.2±4.1%, p<0.002); these differences were greater at night (12.6±16.9 vs. 1.0±1.5%, p<0.0001). Also, the frequency of severe hypoglycemic episodes (<54 mg/dL, duration ≥ 15 minutes) per day was higher for PBH group vs. HC (0.5 vs. 0.1, p<0.002).
Conclusion: Patients with PBH experienced higher GV and greater severity and frequency of hypoglycemia compared to HC, especially at night. The study opened doors for future avenues to explore the potential of CGM technology in assisting PBH patients to recognize early hypoglycemia and prevent severe hypoglycemia.
Reduction in Self-Reported Adverse Events Related to Severe Hypoglycemia in Individuals Using a Predictive Low Glucose System: Results from a Real-World Setting
HARSIMRAN SINGH conducted a study to depict results from a real world setting. This study was presented at the virtual ADA 2020 session. Severe hypoglycemia (SH) is an acute complication of diabetes with potentially adverse clinical and psychosocial consequences. There is limited data published literature in terms of SH-related adverse events (AEs) in patients with type 1 diabetes (PwT1D) in a real-world setting.
The authors recruited PwT1D who had recently started using the Tandem t:slim X2 insulin pump with Basal-IQ Predictive Low Glucose Suspend (PLGS). Amongst other measures, PwT1D reported SH related AEs at baseline and then again at 6 months post-assessment (PA). Fisher’s exact test was used to analyse pre-post differences. Total 665 PwT1D were included in the analysis (19% of these were <18 years old, mean age=37.11 years, female=55.5%, mean HbA1c=7.2%). Overall, 14.9% used multiple daily injections (MDIs) while 85.2% used insulin pumps as baseline therapy method. Nearly 91% of the sample reported using CGM at baseline. At PA, number of participants who reported to have 1 or more paramedic visits due to SH had significantly decreased from 35 to 19 (p<0.001), emergency room (ER) visits dropped to 9 (vs. 39 at baseline, p<0.001), and hospital admissions were reduced to 6 (vs. 24 at baseline, p<0.05) for the entire sample. These differences were observed irrespective of the baseline therapy method (MDIs vs. pump users) although the largest differences were noticed for MDIs (reduction of -9.47% (paramedic visits), -10.53% (ER visits), and -8.42% (hospital admissions). Risk-ratio assessment for AEs overall, per 100 person years showed a drop at PA for all 3 AE categories (paramedic visits, 21.98 vs. 7.33; ER visits, 19.24 vs. 4.27; hospital admissions, 11.30 vs. 2.75).
Conclusion: Remarkable reductions in self-reported SH-related AEs for both pediatric and adult PwT1D were observed with Basal-IQ PLGS technology.
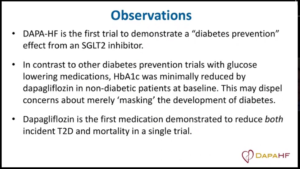
ADA Presidents’ Select Abstract: Effect of Dapagliflozin on the Incidence of Diabetes: A Prespecified Exploratory Analysis from DAPA-HF
SILVIO E. INZUCCHI et.al. presented the study findings for Effect of Dapagliflozin (dapa) on the incidence of Diabetes at the virtual ADA 2020 session. In DAPA-HF, the SGLT2 inhibitor study (i) dapa reduced worsening heart failure (HF) and cardiovascular death in 4744 patients (pts) with HF and reduced ejection fraction (HFrEF.) At baseline only 45% had type 2 diabetes (T2D). The authors evaluated whether dapa reduced the incidence of diabetes in the 55% of pts without T2D. Pts were randomized to dapa 10 mg or placebo and followed for a median of 18.2 months. New-onset T2D was defined as A1c ≥6.5% measured at 2 consecutive study visits post-randomization or investigator-reported new T2D (with the initiation of a glucose-lowering agent.) The effect of dapa on incident T2D was assessed using a Cox proportional hazards model and confirmed with a Fine and Gray competing risk model to account for mortality. Of the 2605 non-T2D pts at baseline, 157 developed T2D on trial, 150 (95.5%) of whom had prediabetes (A1c 5.7-6.4%) (136 [86.6%] using the more restrictive 6.0-6.4% criterion.) Those with incident T2D had a higher mean baseline A1c (6.2 ±0.3 vs. 5.7 ±0.4%; p<0.001), greater BMI (28.5 ±5.9 vs. 27.1 ±5.7 kg/m ; p=0.003), and lower eGFR (61.5 ±17.4 vs. 68.2 ±19.3 ml/min/1.73 m ; p<0.001) than those who remained non diabetic. The results showed that dapa reduced new onset diabetes by 32%: placebo 93/1307 (7.1%) vs. dapa 64/1298 (4.9%); HR 0.68 (95% CI, 0.50-0.94; p=0.019T) (Cox.)
Conclusion: Results were virtually identical using the Fine and Gray model. Diabetes reduction leads to adding a feather in the cap for dapagliflozin benefits.
Comparative Effectiveness of Lifestyle Intervention on Fasting Plasma Glucose in Normal Weight vs. Overweight/Obese Adults with Prediabetes
MANDY K. SALMON, presented a comparative study to show effectiveness of lifestyle intervention on fasting plasma glucose in normal weight vs. Overweight/obese adults with prediabetes at the virtual ADA 2020 session. Normal BMI is observed in almost 1 in 5 U.S adults with prediabetes. It is hypothesized that such individuals develop diabetes through different pathophysiological mechanisms and that methods of prevention may differ in the absence of overweight/obesity. Normal BMI is an exclusion criterion for many diabetes prevention programs and scarce data are available on the effectiveness of lifestyle intervention in normal weight adults with prediabetes. In this study, the author compared the effect of technology-enabled lifestyle health coaching (LHC) on fasting plasma glucose (FPG) in normal weight (BMI 18.5-24.9 kg/m; n = 188), overweight (BMI 25.0-29.9 kg/m; n = 495) and obese (BMI >30.0 kg/m; n = 1,214) adults with prediabetes. Subjects were 1,897 consecutive adults with prediabetes (FPG = 100-125 mg/dl and not taking antidiabetic medication) who completed a baseline and follow-up evaluation as part of an LHC program (mean follow-up = 145 days). LHC included 1-on-1 behaviorally-oriented coaching, predominantly via the telephone and Internet, on exercise, nutrition and weight management. BMI decreased significantly (p <0.001) in the overweight (-0.6±1.1 kg/m) and obese (-1.3±1.8 kg/m) participants but was unchanged (0.0±1.5 kg/m) in the normal weight participants. In contrast, weekly aerobic exercise increased (normal weight = 77±167 min/week increase; overweight = 98±191 min/week increase; and obese = 95±146 min/week increase) and FPG decreased (normal weight = -9±9 mg/dl decrease; overweight = -7±9 mg/dl decrease; and obese = -6±10 mg/dl decrease) significantly (p <0.001) in all 3 groups (p <0.05 for magnitude of decrease in FPG in normal weight versus obese participants). FPG was reduced to <100 mg/dl in 62.4%, 51.7% and 43.6% of the normal weight, overweight and obese participants, respectively.
Conclusion: The study findings suggest that LHC is at least as effective in managing FPG in normal weight adults with prediabetes versus those who are overweight/obese.

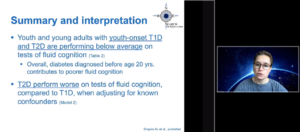
Cognition in Young Adults with Youth-Onset Type 1 and Type 2 Diabetes: The SEARCH for Diabetes in Youth Study
Allison Shapiro presented the SEARCH for diabetes in Youth Study at the virtual ADA 2020 session. In children and adolescents with type 1 (T1D) and type 2 (T2D) diabetes poor cognition has been observed. Differences in cognition between young adults with youth-onset T1D and T2D, however, have not been explored, nor is the effect of shared etiologic processes, e.g., poor glycemic control, on cognition fully understood. Using data from SEARCH for Diabetes in Youth, a multicenter, observational cohort study, the authors compared cognition between young adults with youth-onset T1D and T2D, testing whether glycemic control modified the relationship between diabetes type and cognition. Cognition was assessed via the NIH Toolbox Cognition Battery and age-corrected composite Fluid Cognition scores.
Repeated measures aided in estimating HbA1c of glycemic control. Linear regression modeling was used to test the interaction effect of diabetes type and glycemic control on Fluid Cognition score while controlling for sex, race/ethnicity, waist-height ratio, duration of diabetes, depression, alcohol and drug use, any hypoglycemic episode in the past year, parental highest level of education, household income, and clinic site. The T2D group (n = 254) had significantly lower Fluid Cognition scores, compared to the T1D group (n = 953) (mean [SD] 84.7 [17.3] vs. 95.4 [16.8], p<0.001). Glycemic control modified the relationship between diabetes type and Fluid Cognition scores (interaction p=0.16). Using the model’s interaction estimates, at a HbA1c of 6.5%, the T2D group demonstrated significantly lower Fluid Cognition scores, compared to the T1D group (β = -6.54, 95% CI: -11.52, -1.57, p=0.01). At a HbA1c of 9.5%, Fluid Cognition scores in the T2D group differed to a lesser extent from the T1D group (β = -3.61, 95% CI: -7.16, -0.06, p=0.05). Youth with T2D had poorer cognition then youth with T1D. This effect is more definite at lower HbA1c levels.
Conclusion: The study results suggest that factors unique to youth-onset T2D may impact cognition in this specific diabetes group, warranting further investigation.
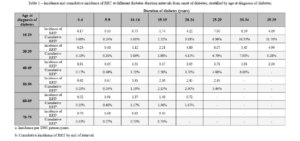
The Association of Age of Onset of Type 2 Diabetes with Long-Term Risk of End Stage Kidney Disease: A National Registry Study
Jedidiah Morton presented The Association of Age of Onset of Type 2 Diabetes with Long-Term Risk of End Stage Kidney Disease at the virtual ADA 2020 session. This study aimed to assess the long-term risk of End-Stage Kidney Disease (ESKD) in type 2 diabetes. The authors included 1,113,201 people with type 2 diabetes registered on the Australian National Diabetes Services Scheme (NDSS) followed from 2002 until 2013. The NDSS was linked to the Australia and New Zealand Dialysis and Transplant Registry and the National Death Index to obtain incident renal replacement therapy (RRT) and death, respectively. Between 2002 and 2013, 7,592 NDSS registrants initiated RRT over 7,839,075 person-years of follow up.
With increasing duration of diabetes the incidence of RRT was also found to be increased. In the first 10-15 years after onset of diabetes, incidence of RRT was highest in those with older age at onset of diabetes. However, over longer durations of diabetes, the cumulative incidence of RRT became higher in those with younger onset diabetes. When “total” incidence of ESKD (RRT and deaths attributed to ESKD without RRT) was considered, the predicted lifetime risks of renal failure (until age 100) were 20.1%, 16.1%, 11.6%, 7.7%, 5.4%, and 4.2% in those with diabetes onset between ages 10-29, 30-39, 40-49, 50-59, 60-69, and 70-79, respectively.
Conclusion: The authors found that the long-term risk of ESKD in type 2 diabetes is high, which disproportionately affects those with younger-onset type 2 diabetes as they are more likely to survive to longer diabetes durations.
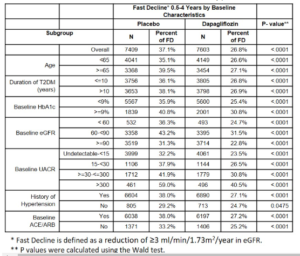
Effect of Dapagliflozin on Risk for Fast Decline in EGFR: Analyses from the DECLARE-TIMI 58 Trial
ITAMAR RAZ et.al. presented his study findings from analyses from the DECLARE 58 trial at the Virtual 80th session of ADA. It is found that SGLT2 inhibitors may lead to short term decrease in eGFR, with later stabilization and long-term reduction in the risk for end stage kidney disease. Fast decline (FD) in eGFR can be defined as a reduction of ≥3 ml/min/1.73m /year and is associated with poor long-term renal prognosis. In this post-hoc analysis we studied the effect of dapagliflozin (dapa) on the risk for FD in the DECLARE-TIMI 58 trial. In DECLARE-TIMI 58, 17,160 patients with T2D and established or increased risk for CVD, with mean baseline eGFR of 85.2 ml/min/1.73m, were randomized to dapa vs. placebo and followed for a median of 4.2 years. The risk for FD was compared between treatment arms. In the time frame of 0.5 years (after stabilization) to 4 years, the proportion of patients with FD was reduced with dapa vs. placebo (26.8% vs. 37.1% respectively, p<0.0001). This observation was persistent in all subgroups assessed (Table). The mean (SD) reduction in eGFR per year was 6.3 (3.7) vs. 0.0 (2.5) ml/min/1.73m /year in the FD (N=4,788) vs. non-FD (N=10,224) patients. The proportion of patients with FD during the entire study period (i.e., 0-4 years) was reduced with dapa vs. placebo as well (33.6% vs. 37.0% respectively, p<0.0001).
Conclusion: In a broad population of patients with T2D and either established or increased risk for CVD, dapagliflozin reduced the risk for FD in eGFR but relatively preserved renal function, irrespective of patients’ baseline characteristics.
A Successful Diabetes Management Model of Care in Long-Term Care Facilities
Sarah et.al. presented the successful diabetes management model of care in long term term care facilities at the 80th Virtual ADA session. The management of diabetes in long-term care (LTC) facilities needs facility staff to perform most diabetes self-care activities on the behalf of the residents. The authors describe a practical model of care to improve diabetes management in LTC facilities. In a span of 4 years, a diabetes management model of care was developed and implemented at six LTC facilities. The components of the program included of: 1) developing individualized curriculum, and educating interdisciplinary staff members, 2) educating patients and families, and 3) developing a practical clinical care algorithm.
Staff members were trained to identify the most likely reasons for hypo- or hyperglycemic episodes and intervention strategies based on the causes. Over 500 LTC staff members were educated and achieved competence during the program implementation. The patients and families received on an average 12.5 education sessions per month in skilled nursing facilities, and 1.5 education sessions per month in nursing homes. A total of 1031 residents were screened to assess risk of hypo- or hyperglycemia on admission to LTC. During the first 2 weeks of stay, hypo- and hyperglycemic episodes occurred in 31.4% and 29.2% of residents respectively. Overall, 245 residents (23.8%) experienced ≥1 episode of hypoglycemia (glucose <70mg/dl). Of those 245 residents, 66.5% had 1 event, 15.5% had 2 events, and 18.0% had ≥3 events. Similarly, 240 residents (23.3%) experienced ≥1 episode of hyperglycemia (≥3 consecutive glucose readings >200 mg/dl) with 63.7% having 1 event, 17.9% with 2 events, and 18.4% having ≥3 events. The most common cause of either hypo- or hyperglycemia was found to be medication related. The hypoglycemia episodes resolved without recurrence in 73-90% cases and interventions reduced the number of events over time.
Conclusion: Staff education can be improved by implementing a practical model of diabetes management in LTC which can lead to improved diabetes management for all residents.
Outcomes of a Digital Diabetes Self-Management Support Program Stratified by A1C
Jonathan et.al. conducted a study to determine the outcomes of a Digital Diabetes Self-Management Support Program Stratified by A1C. This study was presented at the virtual 80th session of ADA. Diabetes Self-Management Support (DSMS) programs are designed to assist people with diabetes as they implement and sustain the behaviors needed to manage their disease. In-person DSMS programs have many attendance barriers that can be mitigated through digital delivery. This study presents at results from the only ADA recognized online digital DSMS program (as of Jan 2020). The program collects diverse Patient Reported Outcomes (PROs) to track patient progress and program impact. This analysis presents digital DSMS program outcomes, focusing on individuals with an A1c >9%, for whom health risk is markedly increased. The study enrolled subjects in a 12-week digital DSMS program and evaluated changes from baseline to program completion. Changes in anxiety, depression, financial toxicity, overall physical and mental health, medication adherence, stress, diabetes distress, body mass index, and A1c were evaluated for cohorts defined by baseline A1c values. Descriptive statistics define frequency and data collected from validated PROs were analyzed to evaluate the outcomes of the digital DSMS program.
Till date 1,349 people with diabetes have participated in the digital DSMS program. 843 of these completed and provided both baseline and 3-month outcome measures. Across all A1c categories, there were significant improvements in physical health, medication adherence, stress, and BMI (p < 0.05). Decreased A1c values at month 3 compared to enrollment (p < 0.01)was seen, people with higher baseline A1c values saw the greatest decrease, A1c ≥ 10% decreased 4.17% (pre:11.32 – post: 7.15%), A1c 9-9.9% decreased 1.34% (pre: 9.29 – post: 7.95%).
Conclusion: The study findings suggested that a digital DSMS program can not only improve glycemic control, but also PROs, and that a digital delivery of a DSMS program is an effective intervention, particularly for individuals with elevated A1c for whom health risks are elevated.
Expanding Diabetes Self-Management Education to Include Chronic Kidney Disease Education
Preetha et.al. conducted a study to determine expansion of Diabetes Self-Management Education to Include Chronic Kidney Disease Education. This study was presented at the Virtual 80th session of ADA. Thirty million Americans have diabetes and 1 in 3 adults with diabetes has chronic kidney disease (CKD). While the Diabetes Self-Management Education and Support (DSMES) curriculum cites CKD risk within one of its eight core content areas, increasing rates of kidney failure among diabetics warrants more robust content devoted to diabetes’ association with CKD.
TMF Health Quality Institute recruited clinical and peer educators in Arkansas, Missouri, Oklahoma, Puerto Rico, and Texas to complete the American Kidney Fund (AKF) Kidney Health Coach (KHC) online training as a means of equipping them with content and strategies to incorporate into DSMES or stand-alone CKD education sessions for Medicare beneficiaries at risk for CKD from October 2017-April 2019. Upon completing KHC, three CKD education delivery methods were piloted: 1) in-person educator-led 2) recorded video shown in class 3) video on-demand. The effectiveness of each method was determined by assessing participant knowledge and comprehension using the AKF Kidney Health Education Session pre/post-test. 615 educators became KHCs and delivered CKD education to a total of 2,250 individuals. Pre/post test scores indicated collective effectiveness among the three delivery methods in increasing understanding of the relationship between CKD and diabetes (relative improvement rate (RIR)= 36.5%). In person CKD education showed most effective in increasing knowledge gain (RIR=38.8%), compared to the recorded video shown in class (RIR=25.3%) and on-demand video (RIR=18.7%) methods.
Conclusion: This study provides evidences for expansion of KHC integration into DSMES, as educating people with diabetes on CKD prevention is critical to reducing the burden of CKD and improving health outcomes, and that an educator-led presentation modality was most effective in improving understanding of CKD.
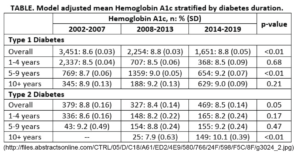
Trends in Glycemic Control among Youth with Diabetes: The Search for Diabetes in Youth Study
Faisal Malik et.al. presented a study to describe temporal trends in glycemic control in youth-onset diabetes at the Virtual 80th ADA session. The study included 6399 SEARCH for Diabetes in Youth participants with diabetes >1 year. Visit data was categorized into 3 time periods: 2002- 2007, 2008-2013, and 2014-2019 and 3 groups of diabetes duration: 1-4, 5-9, and 10+ years. Participants contributed one randomly selected data point to each duration group. Stratified multivariable regression models were used to test differences in hemoglobin A1c (A1c) over time, adjusted for site, age, sex, race/ethnicity, health insurance status, and disease duration, both overall (with repeated measures) and for each duration group.
Among individuals with type 1 diabetes (T1D) estimated mean A1c was different over the three periods with a higher mean A1c in 2014-2019 and 2008-2013 versus 2002-2007 (p<0.01; Table). There was a temporal difference in mean A1c for T1D participants with diabetes for 5-9 years (p<0.01) and for T2D participants with diabetes 10+ years (p<0.01).
Conclusions: Current youth and young adults with T1D in the U.S. have worse glycemic control than earlier cohorts despite of increased availability of diabetes technology, newer therapies, and more aggressive glycemic targets over time. Similarly, participants with T2D diagnosed in childhood and diabetes duration of 10+ years exhibit the temporal trend of worse glycemic control in recent years.
Effect of Dulaglutide on Kidney Function–Related Outcomes in Type 2 Diabetes: Post Hoc Analysis from the REWIND Trial
Jonathan Shaw et.al. conducted a study to determine the effect of Dulaglutide on Kidney Function–Related Outcomes in Type 2 Diabetes. This study was presented at the Virtual 80th ADA session. In participants with type 2 diabetes (T2D) in the REWIND trial, dulaglutide (DU) use for median follow-up of 5.4 years was associated with reduced composite renal outcomes, defined as the first occurrence of new macroalbuminuria, sustained decline in estimated glomerular filtration rate (eGFR) of ≥30%, or chronic renal replacement therapy. The aim of this post-hoc analysis was to evaluate the effect of dulaglutide on renal outcomes related to kidney function that are typically used in renal outcomes studies, defined as the composite endpoint of sustained eGFR decline ≥40%, end-stage renal disease (ESRD), or all cause death. Participants with T2D at cardiovascular (CV) risk were randomized (1:1) to DU 1.5 mg once-weekly or placebo. This post-hoc analysis used Cox proportional hazards modeling for time to first event to determine the risk of renal outcomes. Sensitivity analyses were conducted by replacing the all-cause death component with CV or renal death, or renal death. Treatment groups had similar eGFR (mean±SD: DU=77.2±22.7; placebo=76.6±22.8) at baseline. The incidence rate of the composite endpoint was significantly lower for the DU group compared with placebo (Table).
Conclusion: The study results found that treatment with DU 1.5 mg was associated with a 17% risk reduction in kidney function-related outcomes, suggesting potential delay in progression of diabetic kidney disease in patients with T2D at CV risk.


