Li F, et al. Int J Cardiovasc Imaging. 2020 Jan 1.
Heart failure (HF), a malignant and fatal disease, is a complex clinical syndrome resulting from heart structural remodelling and impaired function in ejecting blood. A key mechanism of HF is cardiac remodelling, which is complex. Myocardial fibrosis, a complicated process resulting in the accumulation of the extracellular matrix (ECM), is an important part of cardiac remodelling. The gold standard for extracellular volume (ECV) quantification relies on the histological analysis of endomyocardial biopsies retrieved from the left ventricle (LV). Li F, et al., conducted a prospective cohort study to evaluate the presence, associations, and prognostic significance of modified Look-Locker inversion recovery (MOLLI)-ECV, likely reflecting diffuse myocardial fibrosis, in HF with reduced ejection fraction (HFrEF) patients.
A total of 45 consecutive HFrEF patients were involved in the study. The target-independent variable was ECV quantified by cardiac magnetic resonance T1 mapping using the MOLLI sequence at baseline. Patients were divided into two group: HFrEF group and control group i.e.10 age- and sex-matched healthy participants with no history of cardiovascular disease. Mean MOLLI–ECV was significantly higher in HFrEF patients versus healthy controls (29.55±1.46% vs. 23.17±1.93%, p < 0.001). Patients were followed for 9 months, during which the primary outcome (cardiac death or first heart failure hospitalization) occurred in 15 patients. By Kaplan–Meier analysis, patients with high MOLLI–ECV ≥ 30.10% had shorter event-free survival than the middle (MOLLI–ECV between 30.10 and 28.60) and low (MOLLI–ECV < 28.60) MOLLI–ECV patients (log-rank, p = 0.0035). Result of fully-adjusted multivariable Cox regression analysis showed MOLLI– ECV was positively associated with the composite outcome of HFrEF patients after adjusting confounders hazard ratio (HR) 2.57, 95% CI (1.09, 6.04). By subgroup analysis, a stronger association was seen in patients with NYHA functional class III–IV, hematocrit < 39.8%, left atrial diameter ≥ 53.5 mm, or without the medical history of MRA or diuretics other than MRA. The p for interaction was < 0.05.
Thus, in HFrEF patients, the relationship between MOLLI–ECV determined by CMR and the composite outcome is linear. High MOLLI–ECV was associated with a higher rate of cardiac mortality and first HF hospitalization in the short term follow up.
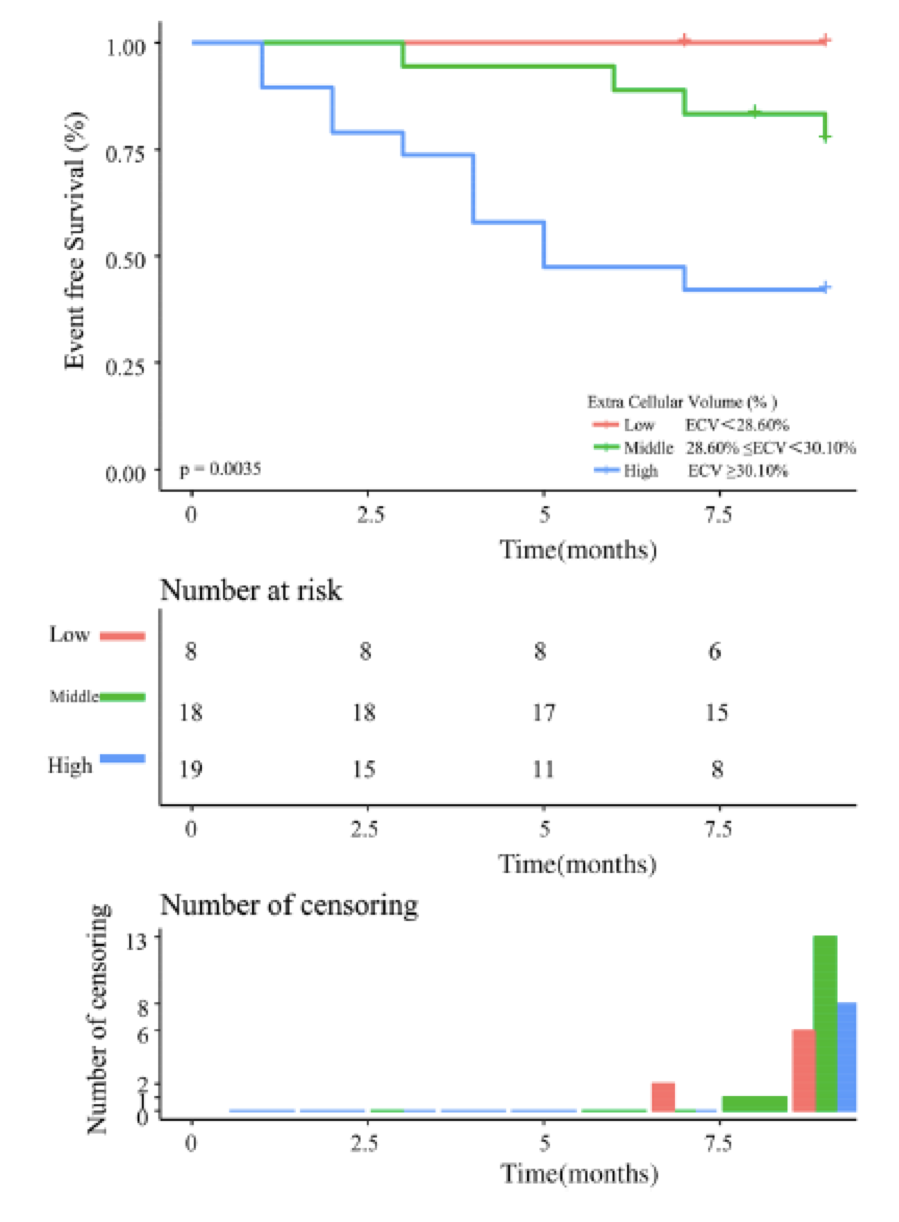
Figure 1: Event-free survival in HFrEF patients according to ECV cutoff

