HIGH ON-TREATMENT PLATELET REACTIVITY WITH CLOPIDOGREL VS TICAGRELOR IN PATIENTS WITH AND WITHOUT CHRONIC KIDNEY DISEASE – A RANDOMIZED CONTROLLED TRIAL
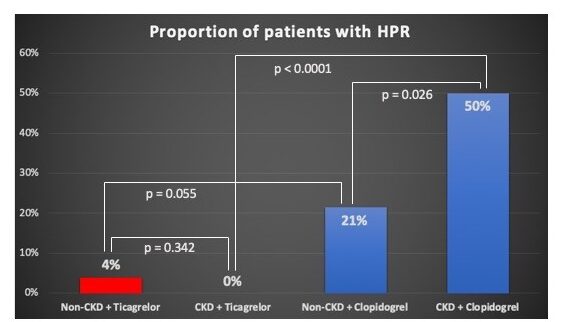
Figure: Proportion HPR in each group
Franci A, et. al., preformed a double-blinded, double-dummy, randomized controlled trial to understand the effect of treatment platelet reactivity with clopidogrel & ticagrelor in patients with or without chronic kidney disease (CKD). Patients with coronary artery disease taking a P2Y12-antagonist who maintain high platelet reactivity (HPR) are at increased risk for ischemic events & CKD patients face a much higher risk for thrombotic events compared to non-CKD pts. The study included 105 patients with previous acute coronary syndrome in the CKD and non-CKD groups & were randomized to treatment with clopidogrel 75 mg QD or ticagrelor 90 mg BID for 1 week.
Results found that high platelet reactivity (HPR) was low with ticagrelor irrespective of kidney function while HPR in CKD patients taking clopidogrel was significantly higher than in non-CKD patients.
TICAGRELOR MONOTHERAPY AFTER PERCUTANEOUS CORONARY INTERVENTION IN HIGH-RISK PATIENTS WITH OR WITHOUT HISTORY OF MYOCARDIAL INFARCTION: A PRESPECIFIED TWILIGHT SUBSTUDY
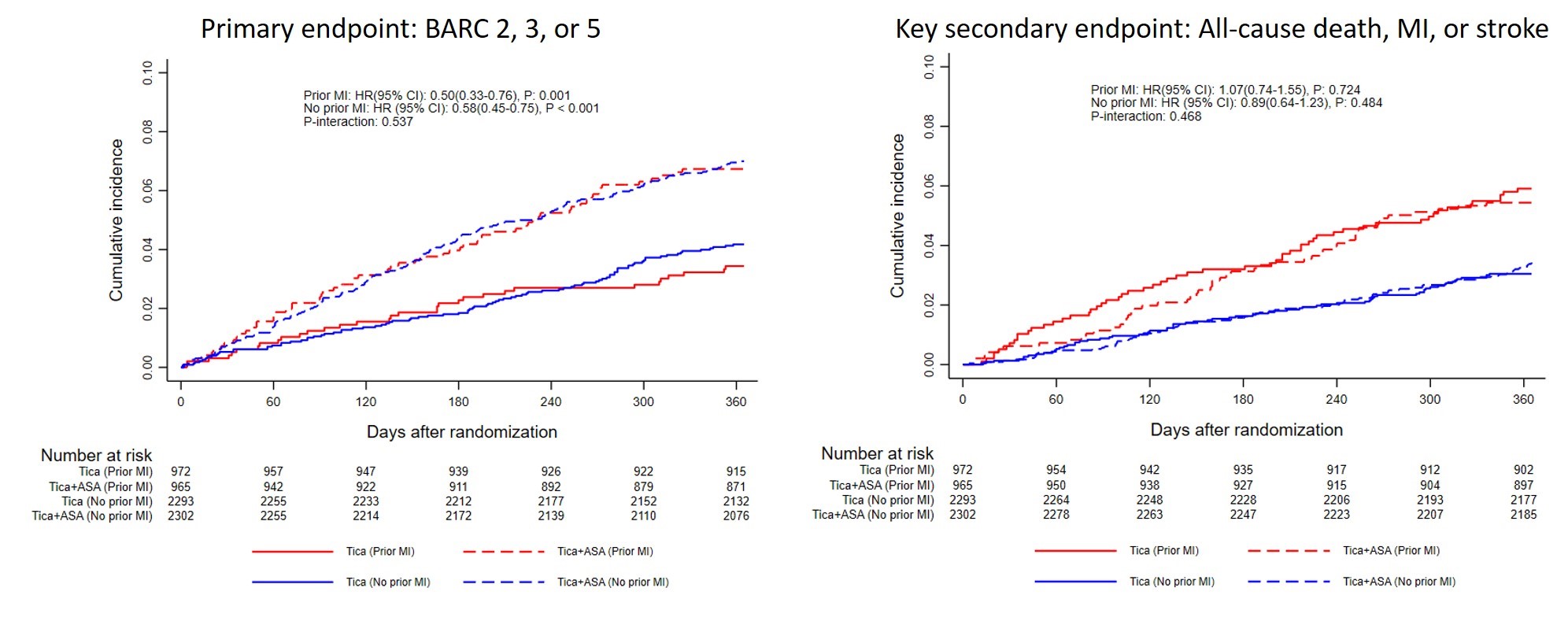
Chiarito M, et. al. conducted a pre-specified sub-analysis from Ticagrelor With Aspirin or Alone in High Risk Patients After Coronary Intervention (TWILIGHT) trial. It assessed the impact of prior MI in treatment effect of ticagrelor monotherapy versus ticagrelor plus aspirin in terms of Bleeding Academic Research Consortium (BARC) type 2, 3, 5 (primary outcome) and of the composite of all-cause death, MI, or stroke (key secondary outcome).
The study included 6532 patients with or without an acute myocardial infarction (MI) who were treated with ticagrelor monotherapy or ticagrelor + aspirin. Results found that patients with a prior MI had a higher rate of ischemic events compared to those without (5.7 vs. 3.2%, p<0.001). Ticagrelor monotherapy reduced BARC 2, 3, or 5 bleeding in patients with prior MI (3.4% vs. 6.7%; hazard ratio (HR) 0.50; 95% confidence interval (CI) 0.33-0.76) to a consistent extent as that seen without prior MI (n = 4595, 4.2% vs. 7.0%; HR 0.58; 95% CI 0.45-0.76; p = 0.54). Rates of death, MI, or stroke among those with and without prior MI) were similar between treatment arms (p = 0.47).
Ticagrelor monotherapy was found to be effective in preventing ischemic events while reduce clinically relevant bleeding as compared to ticagrelor plus aspirin in patients with and without prior MI.
PHARMACODYNAMIC PROFILES OF DUAL ANTIPLATELET THERAPY VERSUS DUAL PATHWAY INHIBITION IN PATIENTS WITH ATHEROSCLEROTIC DISEASE MANIFESTATIONS
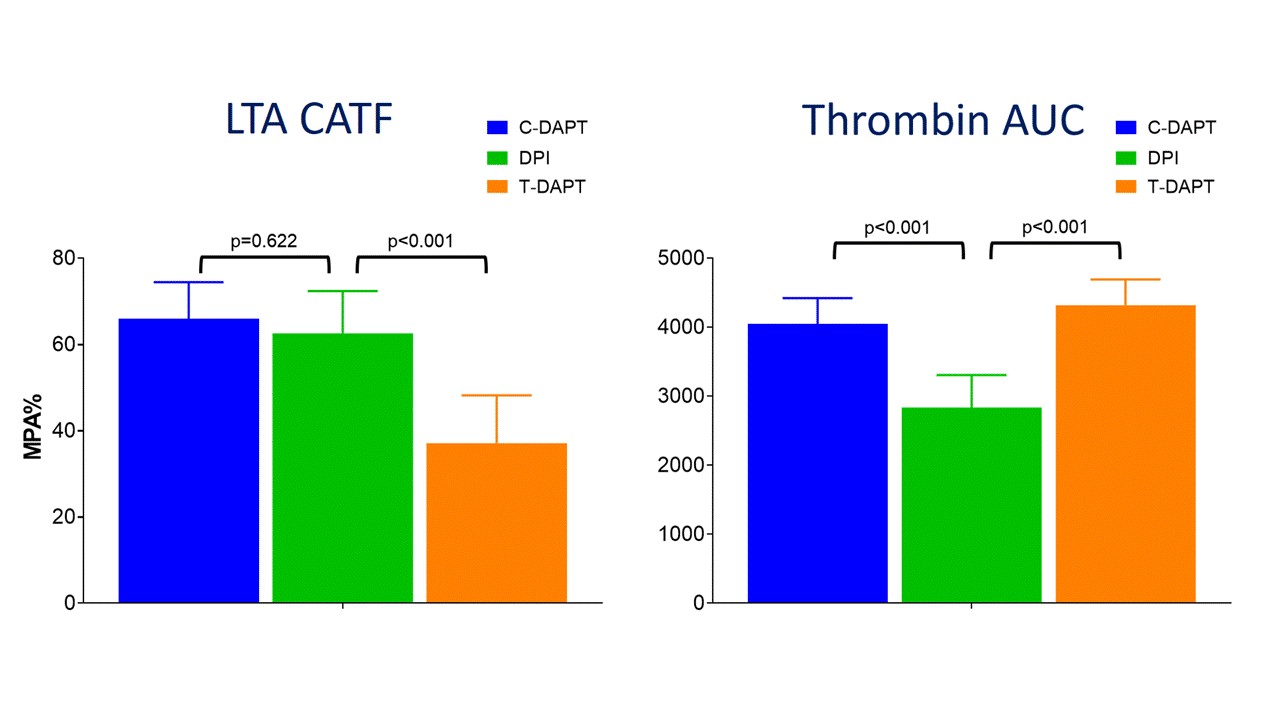
Franchi F, et. al. performed a prospective, open-label, parallel-group cohort study in patients with atherosclerotic disease receiving different antithrombotic regimens. Pharmacodynamic testing was performed in 60 patients with a multitude of assays to describe PD differences between dual antiplatelet therapy (DAPT) with clopidogrel 75mg qd (C-DAPT) or ticagrelor 90mg bid (T-DAPT) vs dual pathway inhibition (DPI) with rivaroxaban 2.5mg bid.
Results found that markers of P2Y reactivity were significantly reduced with C-DAPT and T-DAPT compared with DPI (p<0.001). Tissue factor (TF) induced aggregation was numerically lower with DPI compared with C-DAPT but not with T-DAPT. Global platelet-mediated thrombogenicity induced by collagen-ADP-TF stimuli (CATF) was similar between C- DAPT and DPI however, it reduced with T-DAPT. Markers of thrombin generation, including peak thrombin and total thrombin generated, were reduced with DPI compared with DAPT (p<0.001).
DPI reduces thrombin generation compared with DAPT and has similar effect compared with C-DAPT on global thrombogenicity, which is lower with T-DAPT.
IMPACT OF TICAGRELOR MONOTHERAPY AFTER 3-MONTH DUAL ANTIPLATELET THERAPY IN ACUTE CORONARY SYNDROME BY HIGH BLEEDING RISK: A POST HOC ANALYSIS OF THE RANDOMIZED TICO TRIAL
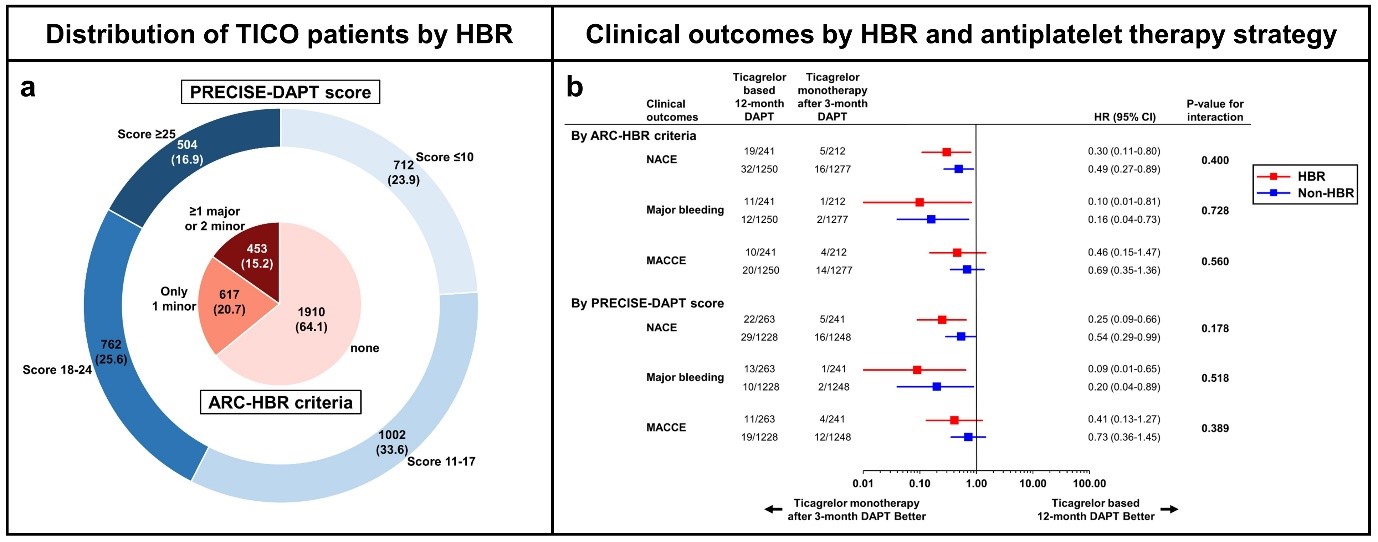
Lee YL, et. al. conducted a post hoc analysis of the TICO trial to identify the impact of ticagrelor monotherapy in patients with high bleeding risk (HBR). The study included 2980 acute coronary syndrome (ACS) patients without adverse events during the first 3 months after intervention.
Results found that 15.2% patients had HBR by ARC-HBR criteria and 16.9% had HBR by PRECISE-DAPT score. The primary outcome rate was higher in HBR vs. non-HBR patients (by ARC-HBR criteria: HR=2.87, 95% CI=1.76-4.69, P<0.001; by PRECISE-DAPT score: HR=3.09, 95% CI=1.92-4.98, P<0.001). Ticagrelor monotherapy after 3-month dual antiplatelet therapy (DAPT) was superior to ticagrelor-based 12-month DAPT regardless of HBR by ARC-HBR criteria, with similar magnitudes of therapy effect (P =0.400) for HBR and non-HBR patients.
Ticagrelor monotherapy after 3-month DAPT was associated with superior clinical outcomes regardless of HBR, with no difference in the therapy effect between HBR and non-HBR ACS patients.
IMPACT OF CLOPIDOGREL VERSUS TICAGRELOR ON CORONARY MICROVASCULAR FUNCTION AND PERIPHERAL ENDOTHELIAL FUNCTION AFTER NON-ST ELEVATION ACUTE CORONARY SYNDROME
Xu J, et. al. performed a prospective randomized study to assess the impact of clopidogrel & ticagrelor on coronary microvascular function and peripheral endothelial function after non-ST elevation acute coronary syndrome (NSTEACS). 108 NSTEACS patients were randomized to clopidogrel (600mg loading then 75mg daily) or ticagrelor (180mg loading then 90mg twice-daily).
It was found that GRACE score, median peak troponin and baseline median IMR in the infarct related artery (IRA) was higher in the clopidogrel compared to the ticagrelor group. Median post-PCI IMR was higher in the clopidogrel compared to the ticagrelor group while pre-discharge median %FMD was lower in the clopidogrel compared to the ticagrelor group (8.1% vs 13.5%, p=0.0002).
In conclusion, ticagrelor resulted in better preservation of coronary microvascular function and improved peripheral endothelial function compared to clopidogrel.
ACUTE CORONARY SYNDROME MANAGEMENT AND OUTCOMES IN VERY ELDERLY PATIENTS – A REAL WORLD EXPERIENCE
Bianco M, et. al. studied the pattern of treatment and outcomes of elderly patient ≥ 80 years old (yo) admitted for acute coronary syndromes (ACS). 193 patients (mean age 84.1 ± 3.5 years), 89 women (46%). 86 (44.6%) patients who presented with STEMI were included in the study.
79 patient with ACS-NSTE and 28 with UA were included and 151 patients underwent PCI. Aspirin was administered in 93.3% patients, clopidogrel in 46.1% patients and ticagrelor in 44% patients. 19.1% patients suffered an in-hospital MACE. 3 (1.6%) had in-hospital TIMI major bleeding while 15 (7.8%) had TIMI minor bleeding. 91.7% were discharged alive with a mean ejection fraction (EF) of 47.7 ± 8.3%. 6.2% patients died of all-cause death after discharge and 23.7% patients required a new hospitalization within six-months.
In very elderly patients ≥ 80 yo routinely treated with invasive strategy and standard dual antiplatelet therapy, a good short-term prognosis was observed irrespectively of age. Six months all-cause mortality was linked to the high age and the number of comorbidities.

