Donal E. JACC Cardiovasc Imaging. 2019 Nov;12(11 Pt 1):2245-2261.
In the general population, AF is independently correlated with a 1.5 to 2-fold elevated risk of all-cause mortality and elevated morbidity. Common cardiovascular risk factors, ischemic cardiomyopathy, valvular heart disease, and heart failure are correlated with left atrial (LA) dilatation and elevated risk of progressing AF. The lack of use of imaging techniques and some remaining pivotal questions is contemplating the requirement for large studies for the long time prescription of anticoagulant therapy including imaging to best manage patients with AF. Donal E et al., conducted a review to discuss the role of multimodality imaging in the assessment and treatment of AF.
In the anteroposterior direction, LA dilatation is commonly asymmetrical and less pronounced. This is the reason why LA volume is the most reliable method to analyse LA dimension and it is estimated by the Simpson’s rule or the area-length ellipsoid methods from biplane 4- and 2- chamber apical views at 2-dimensional (2D) transthoracic echocardiography. Real-time 3D echocardiography might be an attractive substitute for the analysis of atrial volume. The gold-standard method for the detection of SEC or thrombus in the LA and LAA is transesophageal echocardiography (TEE), with a specificity, sensitivity, and accuracy of 100%, 93%, and 99%, respectively. Recently, the use of 3D TEE has conceded 3D reconstruction of the LAA short and long axes and aided a multiplanar approach for the analysis of LAA. Velocities <40 cm/s are correlated with a greater risk of stroke. Atrial function is isolated in 3 components i.e. reservoir function, conduit function, and booster pump function which can be estimated by volumetric and speckle-tracking technics. Myocardial strain imaging widely used to evaluate ventricular function, has also been concerned to evaluate atrial function. (Figure 1)
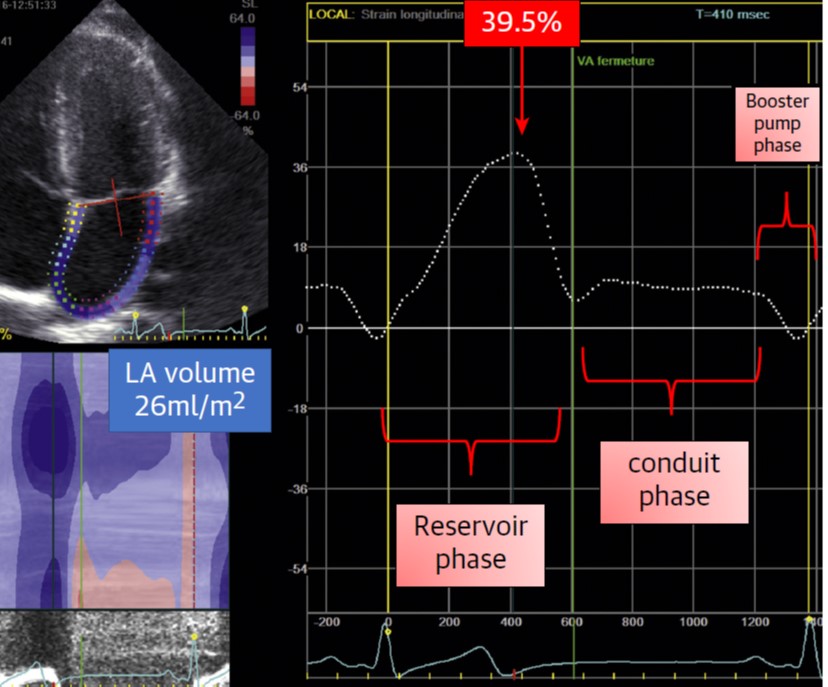
Figure 1: Normal LA Strain Pattern with Normal LA Reservoir Function; LA: left atrial
Atrial function (vitally LA reservoir function) is a predictor of AF incident and reoccurrence and its value appears to be correlated with thromboembolic risk. In the patients of high thromboembolic risk, percutaneous closure of LAA is supposed to be the therapy of choice and indicated contraindication to anticoagulation. Late gadolinium enhancement (LGE) CMR so far has been the main imaging method that facilitates detection, localization, and quantification of LA fibrosis with fairly good histological associates. (Figure 2)
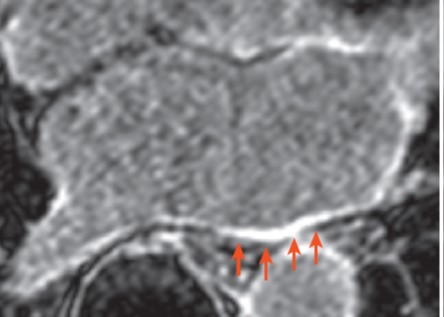
Figure 2: Axial late gadolinium enhancement cardiac magnetic resonance image showing delayed enhancement areas of left atrial posterior wall (arrows) in a patient with persistent atrial fibrillation
It is an important “work-in-progress” image-based approach for best selecting and covering the ablative therapies (AF reoccurrence continuously increased as a function of LGE; LGE >35% has a higher rate of AF reoccurrence in the first year after ablation). LGE CMR could also be useful to specify radiofrequency induced scar of PVs and LA. Post-ablation scar seems to be stable by 3 months post-ablation with a degree of improvement higher than fibrotic remodeling on pre-ablation images. Body surface mapping has arised as a powerful tool to execute non-invasive bedside mapping to recognize AF drivers. The promising strategies to execute AF ablation are drivers’ ablation (with either the FIRM technology or the non-invasive mapping of AF) and substrate modifications with electroanatomic mapping. These techniques established on pre- or periprocedural imaging and focusing patient’s electrical and structural remodelling will permit a “patient-tailored approach” rather than a “phenotype approach” as per the paroxysmal or persistent AF type.
Thus, it was concluded that the evaluation of LA morphology and function is becoming more and more prime in the treatment of patients with AF. LA imaging might also be useful at mild-to-moderate cardioembolic risk for a tailored preventive management of patients.

