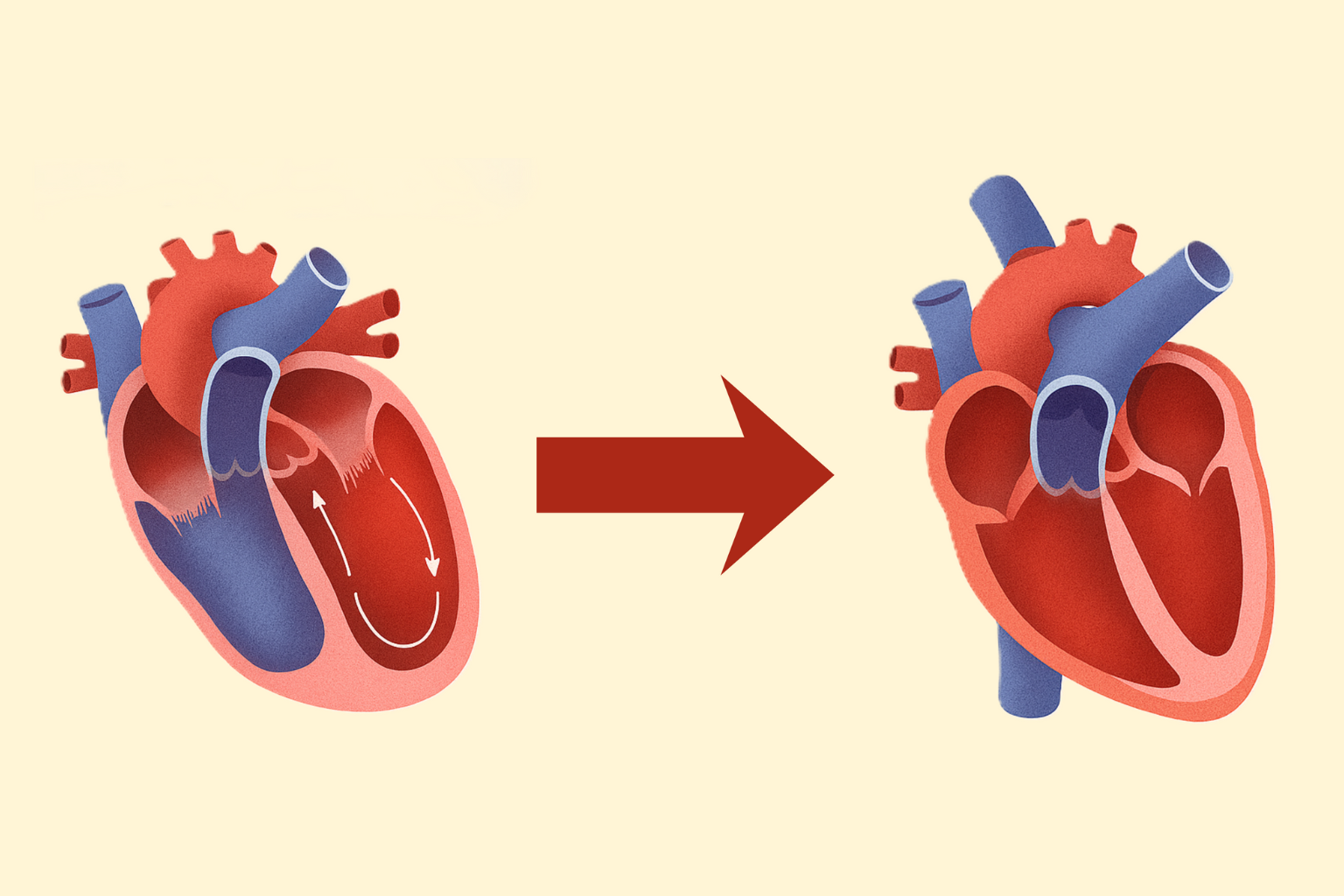
Dilated cardiomyopathy (DCM) is a leading cause of heart failure (HF), with left ventricular reverse remodeling (LVRR) linked to better outcomes, including reduced hospitalizations and mortality. While guideline-directed medical therapy (GDMT) promotes LVRR in HF with reduced ejection fraction (HFrEF), the role of ivabradine—a selective If-channel inhibitor recommended for HFrEF patients in sinus rhythm with resting heart rate (HR) ≥75 bpm despite GDMT—remains underexplored in relation to achieved HR and LVRR. This retrospective study at Severance Hospital (2012-2021) analyzed 255 patients with idiopathic non-ischemic DCM (NIDCM), defined by LVEF ≤35% and dilated left ventricle (LV), excluding ischemic, valvular, or other secondary etiologies via comprehensive diagnostics including cardiac MRI.
Patients were categorized into four groups based on ivabradine use and 1-year achieved HR (cutoff: 70 bpm via ROC analysis for LVRR prediction): Iva−/HR70+ (HR ≥70 bpm without ivabradine), Iva−/HR70− (HR <70 bpm without), Iva+/HR70+ (HR ≥70 bpm with), and Iva+/HR70− (HR <70 bpm with). Baseline characteristics showed median age 56 years, 60.1% male, with ivabradine groups having lower systolic BP, LVEF, and higher baseline HR. GDMT adherence was high (>85% for RAS inhibitors/MRA), but beta-blocker use was lower in ivabradine groups (74-82% vs. 94-95%).
LVRR, defined as ≥10% absolute LVEF increase to >40%, occurred in 46.8% (Iva−/HR70+), 46.6% (Iva−/HR70−), 62.9% (Iva+/HR70+), and 71.1% (Iva+/HR70−) at 1 year (P=0.027). Adjusted odds ratios confirmed higher LVRR likelihood in Iva+/HR70− vs. non-ivabradine groups (OR 4.85 [95% CI 1.97-11.96] vs. Iva−/HR70+; OR 3.60 [1.41-9.18] vs. Iva−/HR70−; P for trend=0.002). Multivariate logistic regression identified male sex (P=0.008), persistent beta-blocker (P=0.004) and ivabradine (P=0.004) adherence, and every 10 bpm HR reduction (OR 1.20 [1.04-1.40], P=0.016) as independent predictors. Sensitivity models supported HR reduction over baseline or categorical achieved HR.
Over a median 730-day follow-up, clinical events (HF hospitalization: 9.4%; CV death: 0.4%) were low, with no significant group differences (log-rank P=0.841). Limitations include retrospective design, potential confounders, and low event rates; SGLT2 inhibitor data were limited due to delayed approval. Findings suggest ivabradine, by achieving HR <70 bpm, enhances LVRR in NIDCM despite lower beta-blocker use, emphasizing intensive GDMT titration. Prospective studies are needed for validation and outcome impacts.

