Insulin is the oldest of the currently available diabetes medications, has the most clinical experience. It is the most effective agent when used in adequate doses to decrease any level of HbA1c to the therapeutic goal. The updated ADA/EASD consensus recommends the use of GLP-1 receptor agonists or SGLT2 inhibitors with proven cardiovascular benefit in patients with type 2 diabetes and established ASCVD or high cardiovascular risk. Several studies have stated that initiation of insulin therapy is often delayed, leading to an increased risk of complications in patients with diabetes. The findings were presented at the EASD Annual Meeting 2025, held from 15 -19 September 2025 in Vienna, Austria.
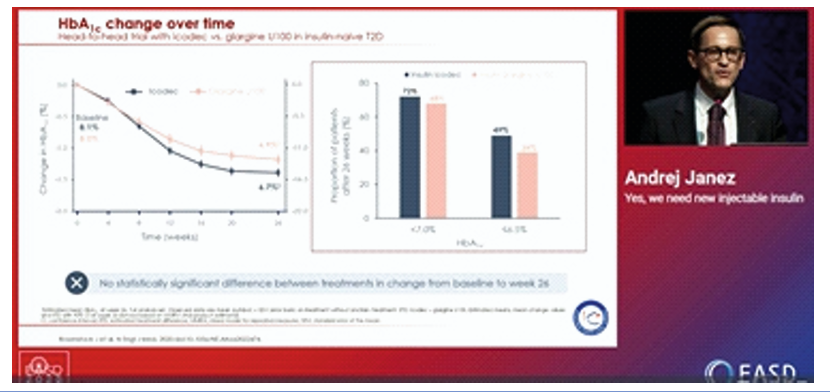
As per Holman et al., NEJM studies (2007 and 2009), the addition of biphasic, prandial, or basal insulin to oral therapy in T2DM significantly reduced HbA1c levels (−1.3%, −1.4%, and −1.2%, resp.), with basal insulin showing lesser hypoglycemic events. Pieber T et al. (2024) study showed that once-daily basal insulins such as glargine and detemir have shorter durations of action, whereas newer formulations like icodec and efsitora enable once-weekly dosing with more stable pharmacokinetic profiles. Icodec has a half life of ~8 days with variable AUC GIR (12.0–16.1%), while Efsitora shows a longer half-life (~19 days) and more stable AUC GIR (13.8–14.7%). In a head-to-head trial (Rosenstock J et al., NEJM 2020) in insulin-naïve T2D patients, once-weekly icodec showed similar HbA1c reduction to daily glargine U100 at 26 weeks (8.1% to 6.7% vs 8.0% to 7.0%), with no significant difference between groups. More patients on icodec achieved HbA1c <7.0% (72% vs 68%) and ≤6.5% (49% vs 39%). Moreover, the duration of hypoglycemia was not longer with Icodec than glargine U100.
A new approach to basal insulin use has been proposed. For insulin-naïve T2D patients, icodec starts at 70U weekly, while efsitora starts at 300U (100U × 3), then 100U from week 2. For insulin-experienced patients, the weekly dose equals the daily dose ×7, plus a one-time loading dose. With icodec, the loading dose is ×1.5 (e.g., 20U daily to 210U first dose, then 140U weekly). With efsitora, the loading dose is ×3 (e.g., 20U daily to 420U first dose, then 140U weekly).
Once-weekly basal insulins such as icodec and efsitora offer a longer duration of action compared to traditional daily insulins, reducing injection burden and simplifying therapy. Emerging strategies include fixed weekly insulin dosing and combined weekly insulin–GLP-1 treatments, which may enhance adherence and improve outcomes in type 2 diabetes.

