Tirzepatide, a dual agonist of the glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptors, has demonstrated superior glycemic control and greater weight reduction compared with GLP-1 receptor agonists alone in patients with type 2 diabetes. Dulaglutide, a GLP-1 receptor agonist, has established cardiovascular benefits in this population. However, the cardiovascular effects of tirzepatide relative to dulaglutide remain unknown.
Chagas disease, caused by Trypanosoma cruzi, is a leading cause of non-ischemic cardiomyopathy in Latin America, affecting 6–7 million people. Despite clear benefit of sacubitril/valsartan over enalapril in HFrEF of other etiologies (PARADIGM-HF trial), its efficacy in Chagas cardiomyopathy remained unknown due to distinct pathophysiology involving chronic inflammation, fibrosis, and microvascular dysfunction.

Tirzepatide, a dual GLP-1/GIP receptor agonist, induces substantial weight loss and cardiometabolic improvements in adults with obesity. However, the SURMOUNT-4 trial demonstrated that most participants regain weight upon discontinuation, raising questions about the durability of associated health benefits. The objective is to evaluate changes in cardiometabolic parameters stratified by the extent of weight regain following tirzepatide withdrawal in the SURMOUNT-4 trial.

Sacubitril/valsartan, an angiotensin receptor-neprilysin inhibitor (ARNI), has revolutionized heart failure with reduced ejection fraction (HFrEF) management since its 2015 approval, demonstrating superior efficacy over ACE inhibitors in the PARADIGM-HF trial. However, real-world safety concerns, particularly regarding angioedema and renal effects, necessitate post-marketing surveillance. This study conducts a disproportionality analysis using the FDA Adverse Event Reporting System (FAERS) database to compare adverse drug events (ADEs) between sacubitril/valsartan and valsartan monotherapy, aiming to detect pharmacovigilance signals and guide clinical decision-making.
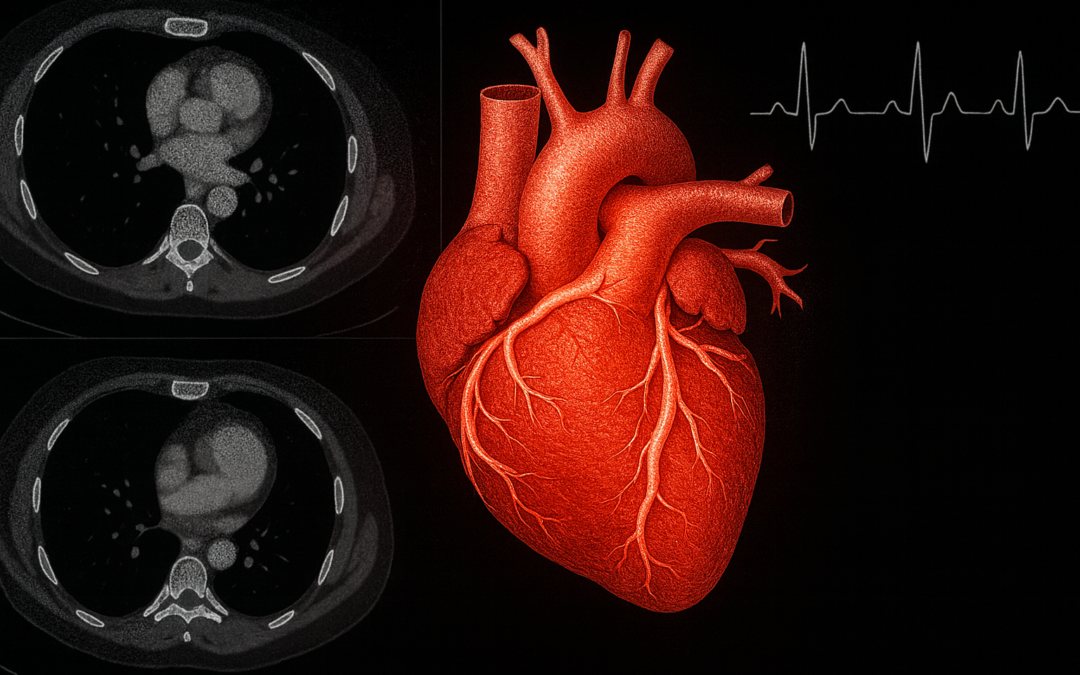
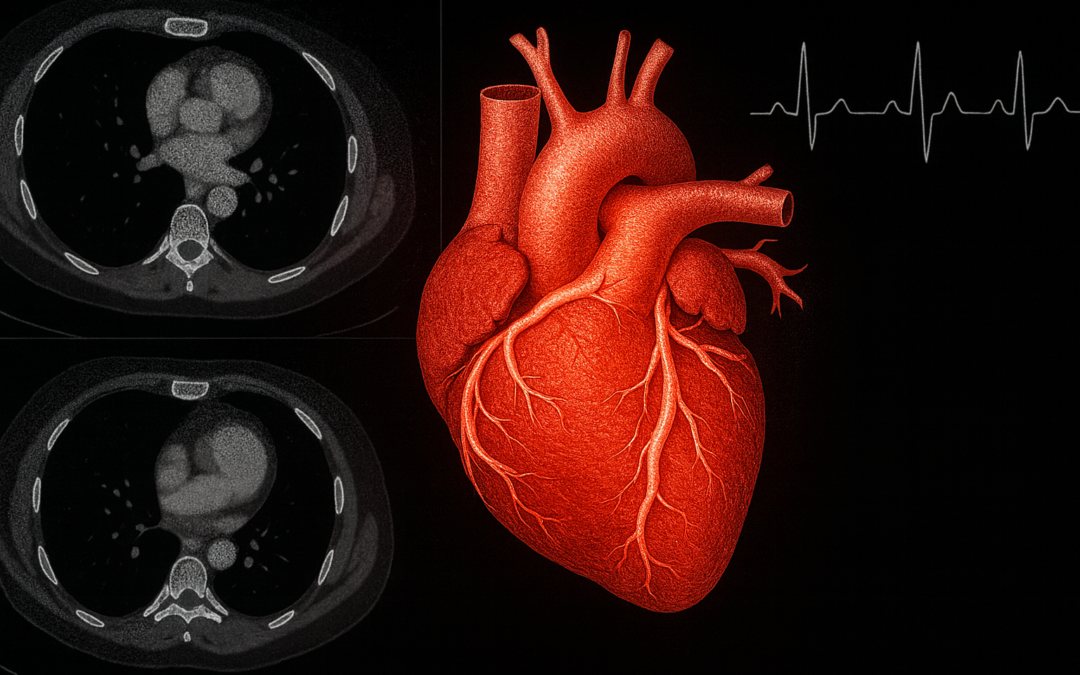
Advanced cardiovascular imaging plays a pivotal role in diagnosing, risk-stratifying, and managing a spectrum of cardiac conditions, from ischemic heart disease to cardiomyopathies and valvular disorders. However, rapid technological evolution—spanning echocardiography (echo), cardiovascular computed tomography (CCT), cardiovascular magnetic resonance (CMR), and nuclear cardiology—demands rigorous, standardized training to ensure competency and patient safety. The 2025 Advanced Training Statement on Advanced Cardiovascular Imaging, jointly authored by the American College of Cardiology (ACC), American Heart Association (AHA), American Society of Echocardiography (ASE), American Society of Nuclear Cardiology (ASNC), Society of Cardiovascular Computed Tomography (SCCT), and Society for Cardiovascular Magnetic Resonance (SCMR), and issued by the ACC Competency Management Committee, addresses this need by updating prior frameworks to reflect contemporary practice.
Although evolocumab, a PCSK9 inhibitor, reduces major adverse cardiovascular events (MACE) in patients with prior myocardial infarction (MI), stroke, or peripheral artery disease, its efficacy in preventing first cardiovascular events in patients without such history remained uncertain.