Diabetes mellitus is a chronic metabolic disorder with high global prevalence and considerable risk of long-term complications if glucose levels remain uncontrolled. Mobile health (mHealth) interventions—leveraging smartphones, SMS messaging, and telehealth technologies—offer scalable tools for diabetes self-management, patient engagement, and clinical monitoring. This systematic review and meta-analysis aimed to comprehensively evaluate both the clinical efficacy and cost-effectiveness of mHealth interventions in diabetes care.

Heart failure (HF) represents a prevalent and prognostically important complication in individuals with type 2 diabetes (T2D), contributing substantially to morbidity and mortality. Although glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have shown cardiovascular benefit in T2D, the impact of the once-daily oral semaglutide formulation on HF outcomes has not been fully characterized. The SOUL trial was a multinational, randomized, double-blind, placebo-controlled cardiovascular outcomes study in adults with T2D and atherosclerotic cardiovascular disease (ASCVD) and/or chronic kidney disease (CKD), originally designed to assess major adverse cardiovascular events (MACE). This secondary analysis evaluates the effect of oral semaglutide on HF outcomes according to HF status at baseline.

Tirzepatide, a dual agonist of the glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptors, has demonstrated superior glycemic control and greater weight reduction compared with GLP-1 receptor agonists alone in patients with type 2 diabetes. Dulaglutide, a GLP-1 receptor agonist, has established cardiovascular benefits in this population. However, the cardiovascular effects of tirzepatide relative to dulaglutide remain unknown.

The American Diabetes Association (ADA) Standards of Care in Diabetes—2026, published as a supplement to Diabetes Care (Volume 49, January 2026), offers a comprehensive, evidence-graded framework (A–E) for healthcare professionals managing diabetes across diverse populations, including type 1, type 2, gestational, monogenic, and special cases like cystic fibrosis- or immunotherapy-related diabetes. Developed by the Professional Practice Committee through systematic reviews (June 2024–July 2025), the document adopts person-first, empowering language; updates evidence levels; and incorporates endorsements from global societies. Targeting primary care providers, specialists, educators, policymakers, and patients, it stresses shared decision-making, social determinants of health (SDOH), and telehealth to mitigate access barriers, such as insulin cost caps under the Inflation Reduction Act ($35/month) and 15–19% nonadherence due to affordability.
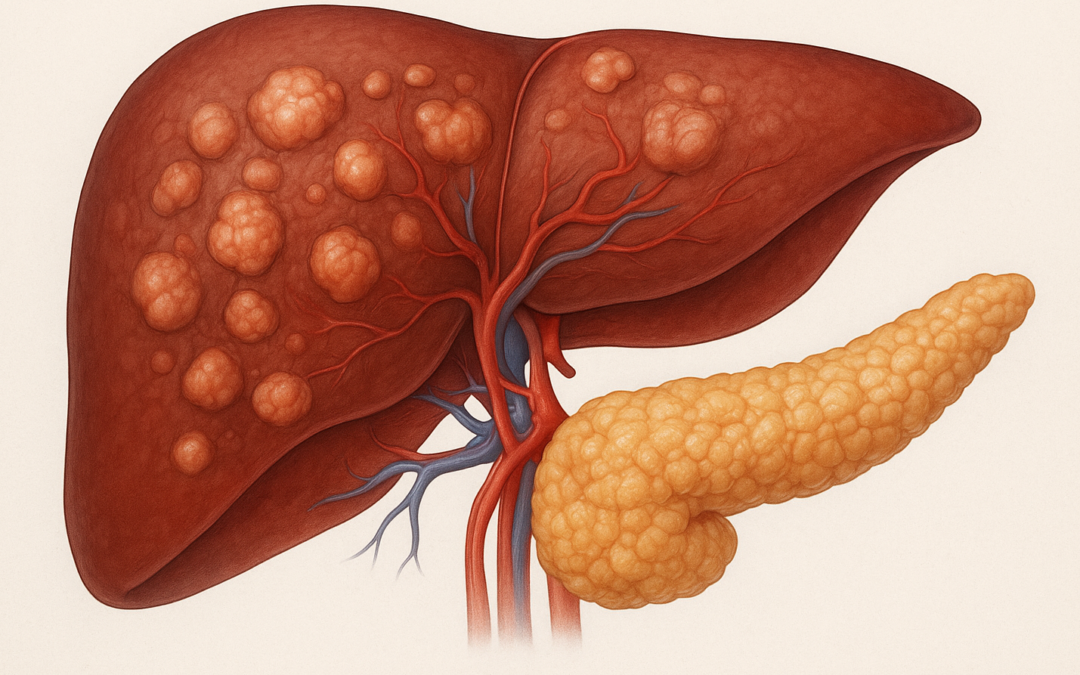
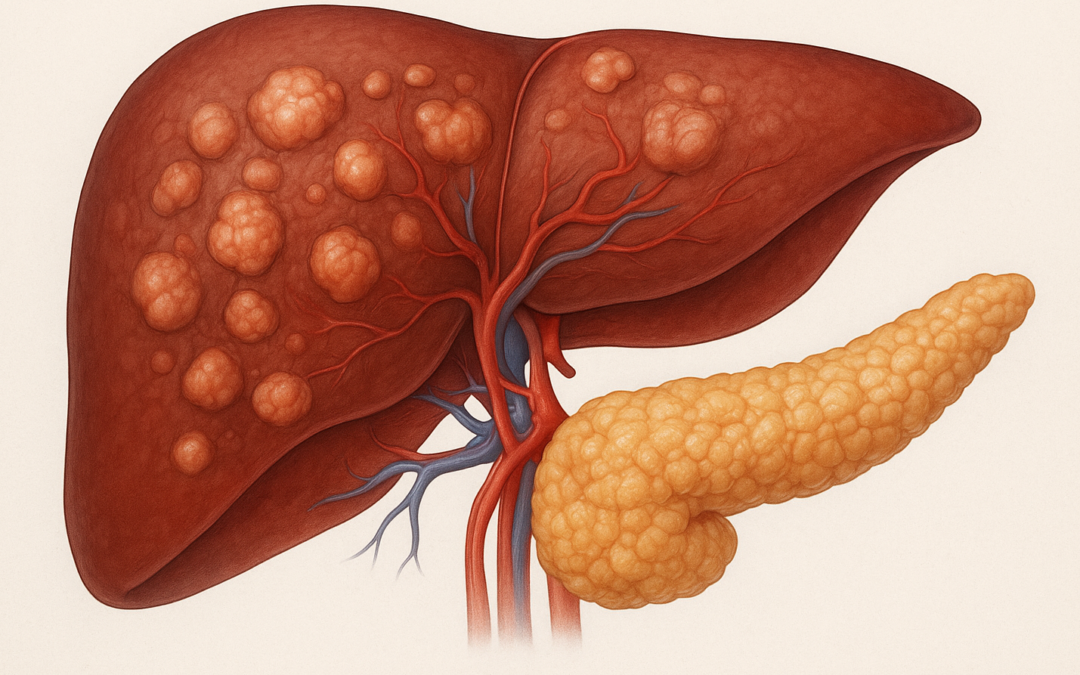
Type 2 diabetes (T2D) in Asian Indians is characterized by high ectopic fat deposition in liver and pancreas, elevated Fetuin-A (an insulin resistance mediator), and hepatic fibrosis risk. While SGLT2 inhibitors like Dapagliflozin (DAPA) reduce hepatic and pancreatic fat, Metformin’s effects on these parameters, especially Fetuin-A and fibrosis, remain underexplored in this population.

Innovent Biologics, a leading Chinese biopharmaceutical firm focused on oncology, metabolic, and autoimmune therapies, announced positive topline results from its fourth phase 3 trial, DREAMS-3 (NCT06184568), evaluating mazdutide (Xinermei®)—a once-weekly subcutaneous GLP-1 and glucagon (GCG) dual receptor agonist licensed exclusively from Eli Lilly for development in China. Originally discovered by Lilly, mazdutide targets both receptors to enhance glycemic control and promote significant weight loss, addressing the intertwined epidemics of T2D and obesity in China, where over 140 million adults live with T2D and obesity rates exceed 16%.