Disertori M. J Cardiol. 2020 Feb;75(2):148-154.
The risk of total mortality (TM) and sudden cardiac death (SCD) has substantially and sequentially reduced in heart failure (HF) patients over the past 20 years with new therapies. However, the guidelines for implantable cardioverter-defibrillator (ICD) therapy have endured unchanged in primary prevention of SCD. This suggested ICD therapy is based only on left ventricular ejection fraction (EF) values and NYHA functional class symptoms in patients with HF of both ischemic and non-ischemic origin. However, current guidelines recommendations for ICD are based on randomized controlled trials (RCTs) carried out in the past three decades and their meta-analyses. Thus, Disertori M et al., conducted a study to underline prospective changes over time in ICD clinical advantage in primary prevention of sudden cardiac death and to evaluate the temporal trends of RCT risk of mortality effects in this time frame.
The MEDLINE and the Cochrane Library electronic databases were searched and recognized 1128 appropriate studies from January 1985 to September 2018. A total of 1113 studies were excluded after reading title and abstract, finally 7 RCTs were incorporated in this analysis. The efficiency of ICD therapy was estimated in the ICD arm with respect to the control in terms of the RR and RD of SCD. The correlation among the randomization starting year of the trials and the AER of SCD and TM in the control arm, the RR and RD of SCD in ICD patients versus controls, the NNT of TM at 3 years was assessed by weighted univariate linear regression analysis. The follow-up period was ≥20 months. AER of SCD estimated the baseline risk for SCD in the control arms of the RCTs, exhibited a successive decrease over time (from 5.7–7.8% in the MADIT and MUSTT trials to 2.5–3.0% in the DEFINITE and SCD-HeFT trials to 1.5% in the DANISH trial) (Fig. 1).
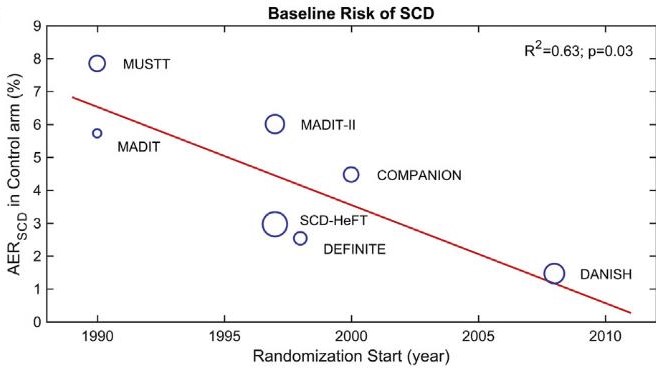
Figure 1: Temporal evolution of the baseline risk of sudden cardiac death (SCD)
The temporal evolution of the relative risk of SCD for ICD versus control arms, exhibited a successive increase in SCD over time, indicative of the fraction of ICD unresponsive patients, (from 24.5% in the MADIT to 37.7% in the MADITII to 52.5% in the DANISH trial) and linear regression evaluation exhibited a statistically substantial enhancement of the RR with an increment of 1.4% per calendar year. (p = 0.04) (Fig. 2)
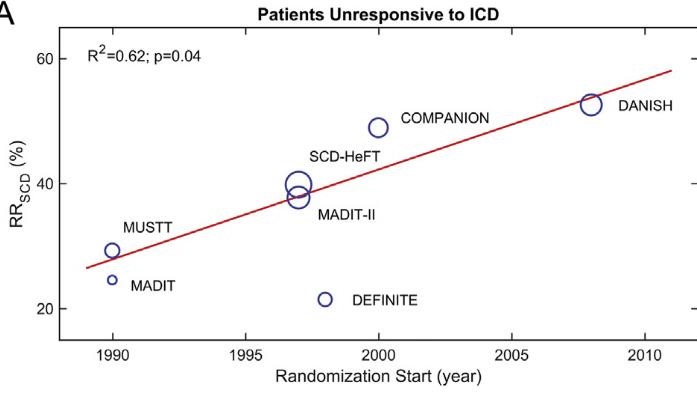
Figure 2: The relative risk (RR) of sudden cardiac death (SCD) in ICD versus control patients
NNT values exhibited a successive increase over time, (from 4–5 in the MADIT and MUSTT trials, to 11 in the MADIT-II trial, to 20 in the SCD-HeFT trial and to 45 in the DANISH trial). Altogether, linear regression evaluation showed a statistically substantial increase in the NNT with an increment of 2 per calendar year, indicating a successive decline of ICD clinical advantage over time. (p < 0.01) (Fig. 3)
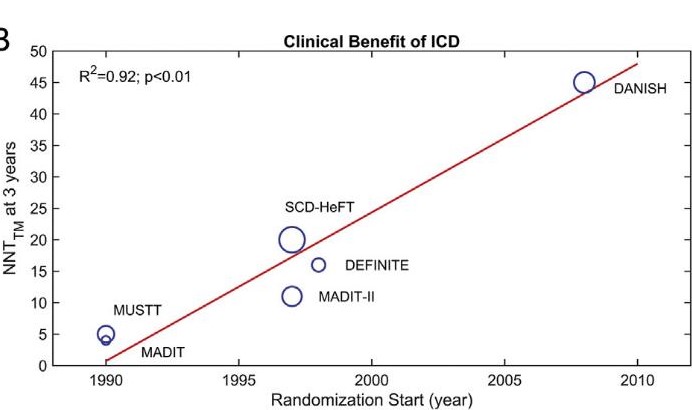
Figure 3: The number needed to treat (NNT) for total mortality (TM) at 3 years
Thus, it was concluded that the clinical advantage of ICD has significantly and successively declined over time as per the current guidelines because of the reduction in sudden cardiac death risk and increase of ICD unresponsive patients.
NYHA: New York Heart Association; RCT: Randomized Controlled Trial; AER: Annualized Event Rate; TM: Total Mortality; NNT: Number Needed to Treat; RR: Relative Risk; RD: Risk Difference

