A major French study published in the European Heart Journal reveals that two out of five patients with heart failure do not see a cardiologist even once a year—a gap linked to significantly higher mortality rates. The study, involving over 655,000 patients and presented at the Heart Failure Congress 2025, found that patients who had at least one cardiologist visit annually were 24% less likely to die in the following year.

A recent study presented at Heart Failure 2025, a congress of the European Society of Cardiology (ESC), highlights the promising performance of an artificial intelligence (AI)-enabled electrocardiogram (ECG) algorithm in detecting early signs of heart failure in Kenya. The study specifically focused on identifying left ventricular systolic dysfunction (LVSD), a precursor to heart failure, in a resource-limited setting where access to echocardiography—the gold standard diagnostic tool—is limited.
A pharmaceutically manufactured cannabidiol (CBD) formulation demonstrated a favorable cardiac safety profile in a prospective, placebo-controlled trial involving patients hospitalized with non-critical COVID-19 and at high risk for cardiovascular events. The findings were presented at the Heart Failure 2025 congress of the European Society of Cardiology (ESC) on 17 May 2025 in Belgrade, Serbia.
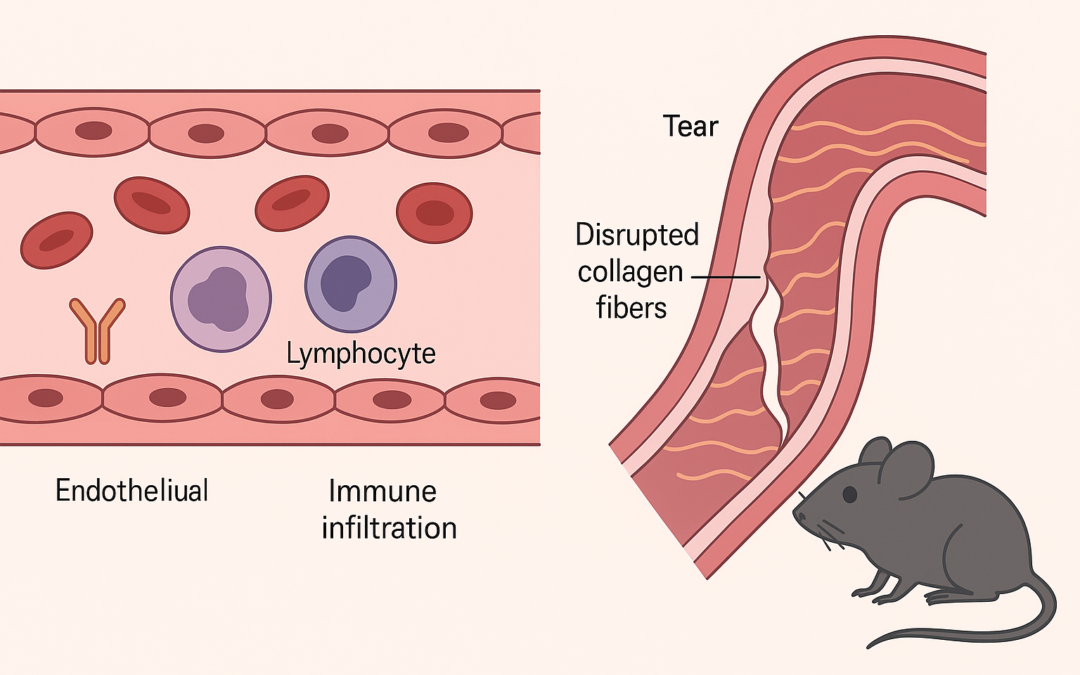
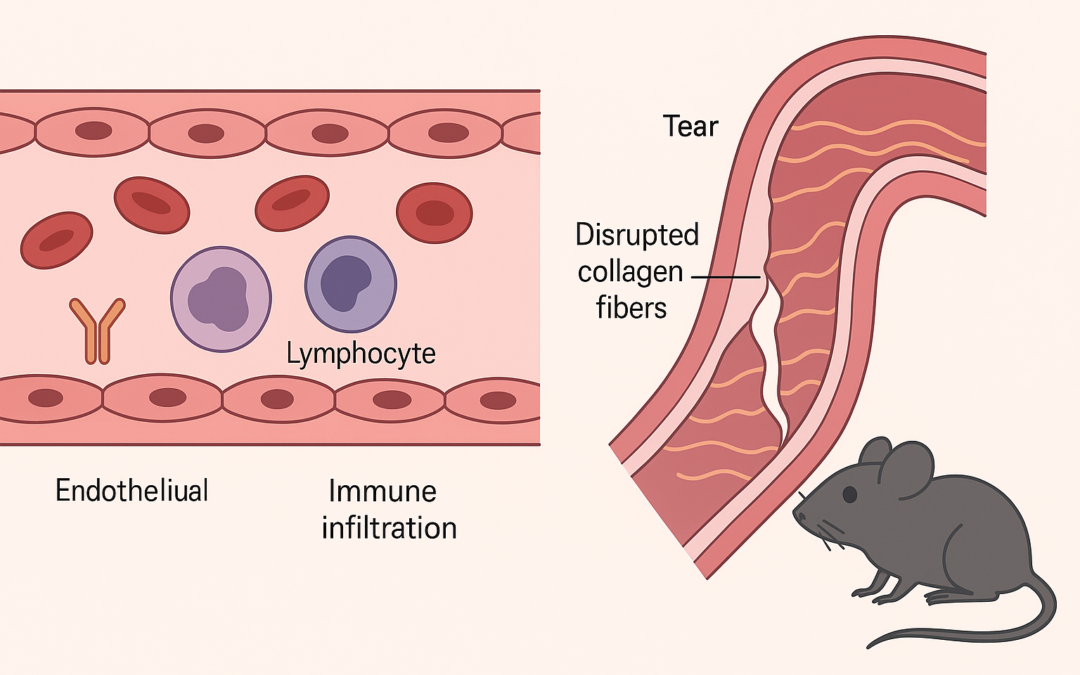
The study presents a novel mouse model for spontaneous aortic dissection (AD), developed by introducing a patient-derived FBN1 gene variant (Gly234Asp) using CRISPR/Cas9. This mutation, identified in a family with nonsyndromic AD, leads to early-onset, rapidly progressing aortic dissection in homozygous mutant mice, with a 50% mortality rate by five weeks of age. The mutant mice exhibit multiple intimomedial tears in the ascending aorta, mimicking human pathology. The research identifies early abnormalities in endothelial cells (ECs), such as misalignment with blood flow and upregulation of adhesion molecules (VCAM-1 and ICAM-1), contributing to immune cell recruitment.
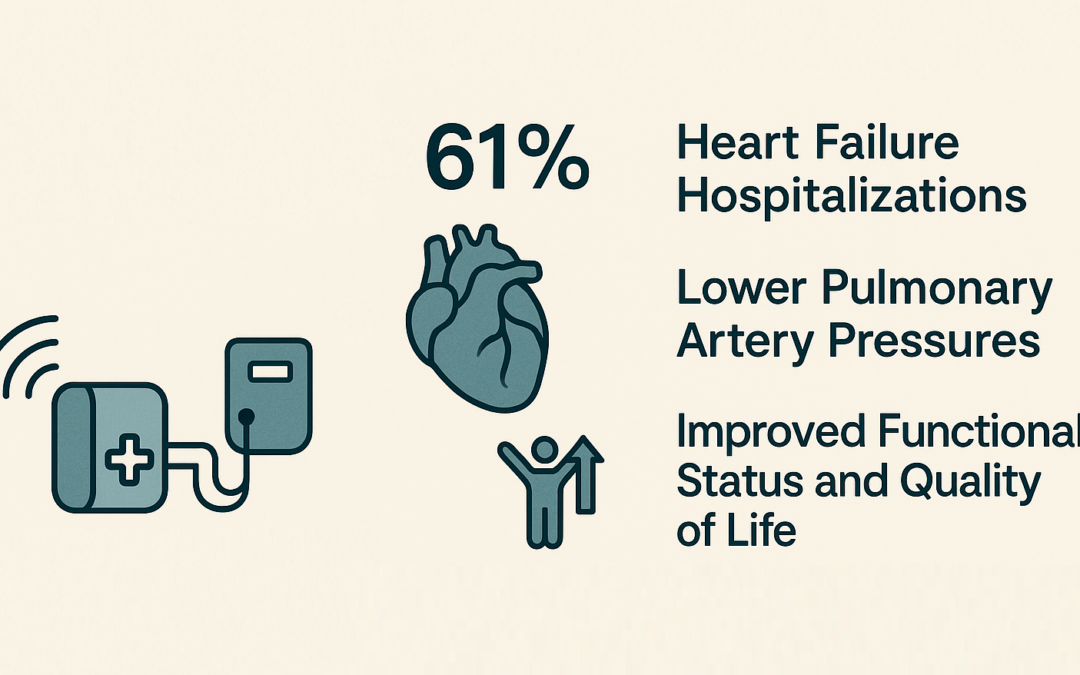
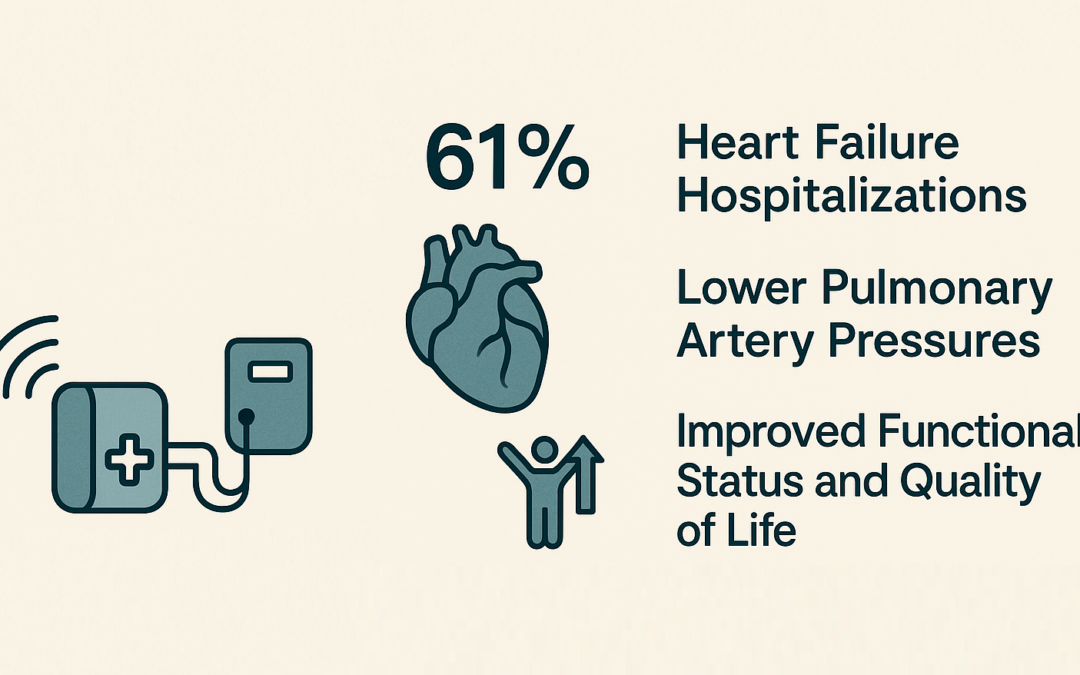
This systematic review and meta-analysis evaluates the effectiveness of pulmonary artery pressure (PAP)-guided management using the CardioMEMS Heart Failure System in patients with heart failure (HF) outside the controlled settings of randomized clinical trials. The study aims to assess real-world evidence regarding the system’s impact on key clinical outcomes, particularly heart failure hospitalizations (HFHs), functional status, and quality of life.
The study investigates the long-term cardiovascular and mortality risks associated with adult-onset type 1 diabetes (T1D), especially in individuals diagnosed at age 40 or older, using data from over 10,000 people with T1D in Sweden. It compares them with patients with type 2 diabetes (T2D) and over half a million diabetes-free controls, tracking outcomes from 2005 to 2022.