Isbister JC. Int J Cardiol. 2021 Feb 1;324:96-101.
Sudden cardiac arrest (SCA) is most frequent in those aged over 35 years because of coronary artery disease however genetic heart diseases represent a significant cause in young patients. Current guidelines (2011 and 2013), suggest that targeted genetic testing only be executed in SCA survivors if a specific genetic condition is suspected. The role of genetic testing needs reappraisal in the treatment of clinically-idiopathic SCA survivors with the advances in genetic testing technology, elevating accessibility of broad genetic evaluation and standardisation of variant classification standard. Thus, Isbister JC, conducted a study to analyse the output of broad genetic testing in clinically-idiopathic SCA survivors and evaluate the prospective diagnostic utility of such multi-phenotype testing in this group.
A single centre study of clinically-idiopathic SCA survivors subjected to assessment of genes known to be correlated with either cardiomyopathy or primary arrhythmia syndromes, after assigning to a specialised genetic heart disease clinic in Sydney, Australia from 1997 to 2019. Comprehensive review of clinical records, analyses and reappraisal of genetic data was executed as per the current variant classification criteria.
61% patients (n = 22) were male from the 36 idiopathic SCA survivors. 21 (58%) SCA survivors were aged ≤35 years at the time of their arrest and the mean age over the group was 36.9 ± 16.9 years (Figure 1A). Arrests most frequently arised in the home (37%, n=13) and nearly two-thirds of incidents in the rest or sleep (65%, n = 22, Figure 1B).
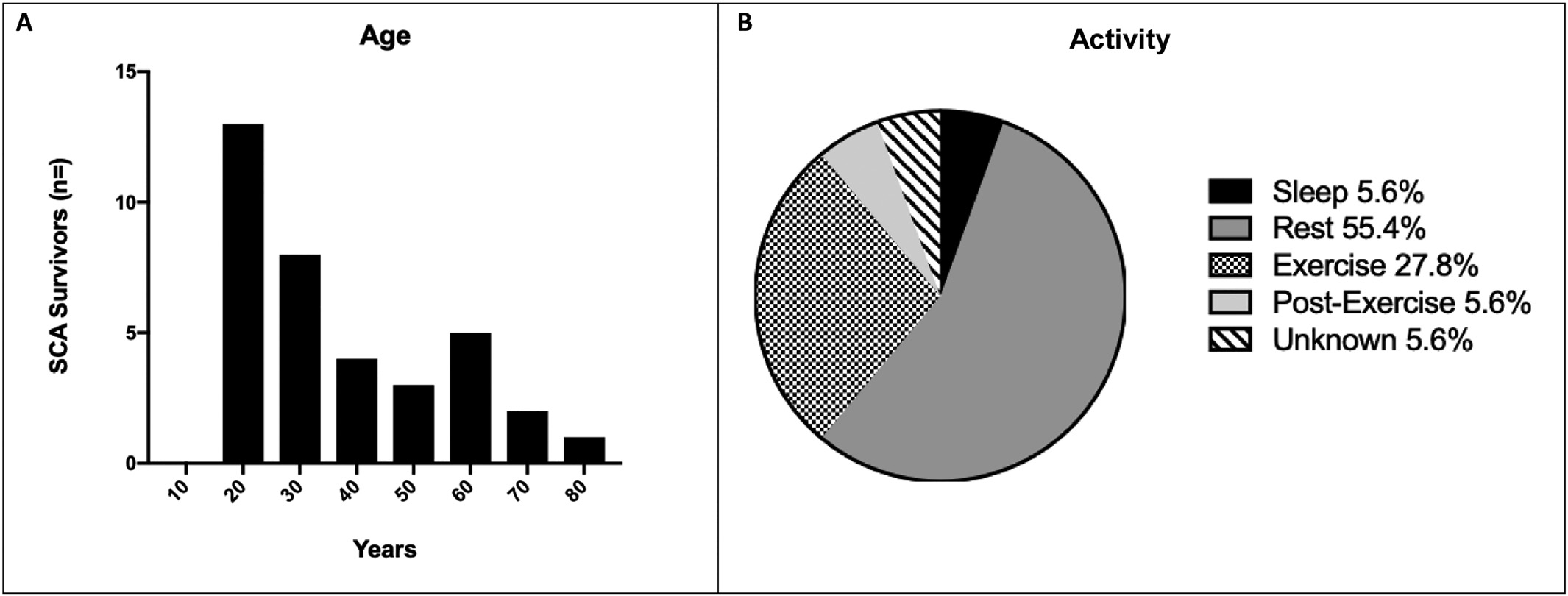
Figure 1: Age and activity at time of SCA. A) Histogram of age at time of SCA and B) Activity at time of SCA.
22% (n=8/36) clinically-idiopathic SCA survivors (mean age 36.9±16.9 years, 61% male) showed a disease-causing variant recognised on broad genetic testing. Of these, a higher proportion of disease-causing variants (ACTN2, DES, DSP, MYBPC3, MYH7, PKP2) resided in those aged ≤35 years [88% (n =7)] than those aged >35 years [12% (n=1)] in spite of structurally normal hearts or sub-diagnostic structural changes at the time of arrest, so-called “concealed cardiomyopathy”. Only one SCA survivor showed a variant recognised in a channelopathy correlated gene.
Thus, it was concluded that in 22% of SCA survivors, genetic testing can recognise a cause of arrest where clinical analyses failed to disclose a diagnosis. The most of causative variants were existed in cardiomyopathy genes in the absence of structural disease. Concealed cardiomyopathy is an under-recognised cause of clinically-idiopathic SCA and can be recognised with broad, multiphenotype genetic evaluation. More comprehensive cascade testing and longer follow-up of probands as well as genotype-positive relatives will be beneficial to better understand the natural history of concealed cardiomyopathy and recognise factors that impact disease development.

