Low-dose aspirin is often used to prevent superimposed preeclampsia in women with chronic hypertension, but its effectiveness remains limited. Factors such as dosage, timing of therapy initiation, timing of ingestion, and adherence may contribute to this reduced efficacy, yet these aspects are underexplored and yield conflicting results. Understanding the interplay of these factors and the underlying pathogenesis is critical to optimizing aspirin therapy.
Diffuse interstitial fibrosis is a key contributor to adverse outcomes in hypertensive heart disease and may be reversible. Sacubitril/valsartan, a combined angiotensin receptor- neprilysin inhibitor, may offer superior anti-fibrotic effects compared to valsartan alone. The REVERSE-LVH phase 2 open-label trial (clinicaltrials.gov NCT: 03553810), funded by the National Medical Research Council of Singapore, investigated the myocardial benefits of sacubitril/valsartan in patients with essential hypertension and left ventricular hypertrophy (LVH).
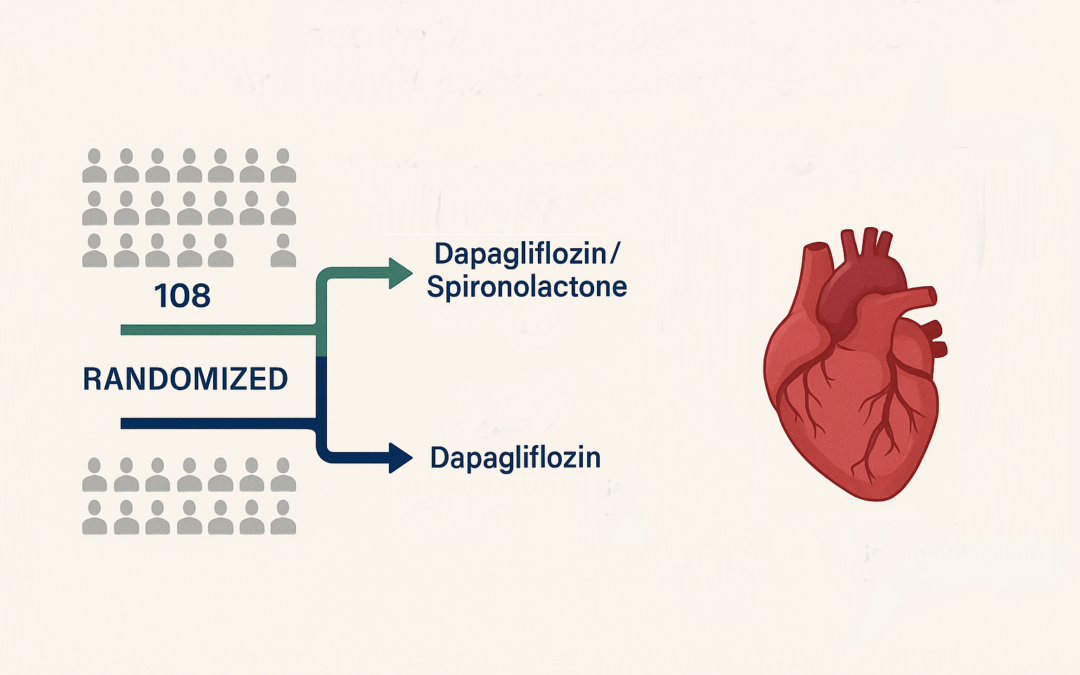
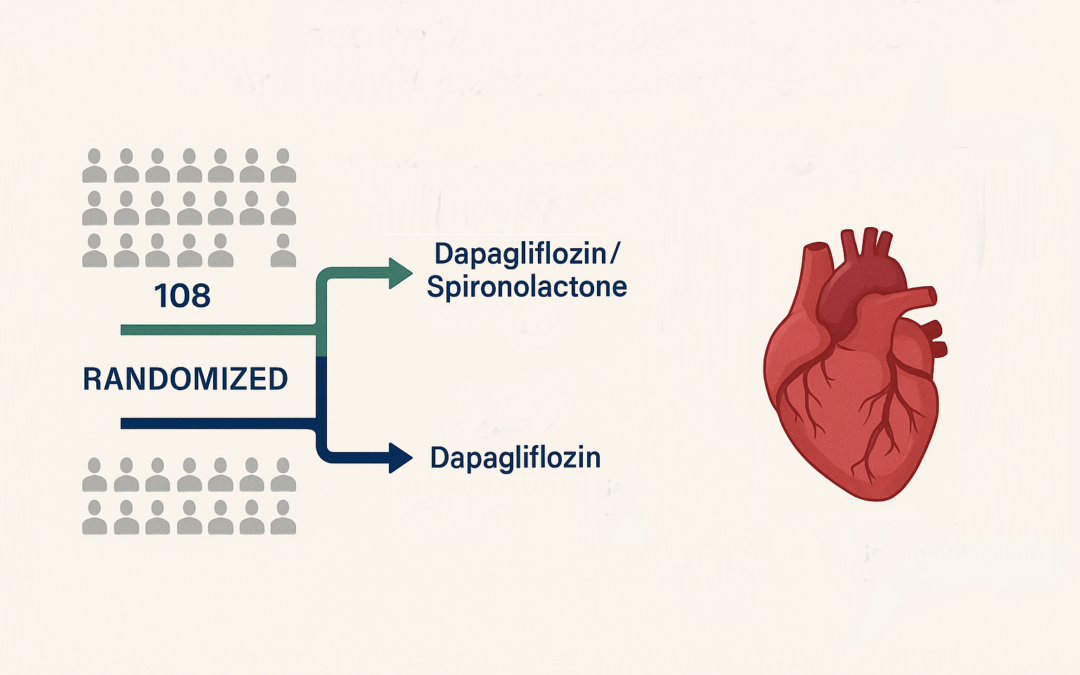
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) and mineralocorticoid receptor antagonists have individually improved outcomes in heart failure with preserved ejection fraction (HFpEF) or mildly reduced ejection fraction (HFmrEF). However, the efficacy and safety of combining these agents remain untested in randomized trials, necessitating dedicated studies to evaluate potential synergistic benefits.

Hypertension, a prevalent lifestyle disorder, targets a blood pressure (BP) of less than 140/90 mmHg, with amlodipine, a calcium channel blocker, serving as a first-line treatment. Understanding its usage patterns, effectiveness, and tolerability, particularly in diverse populations with comorbidities, is critical for optimizing therapeutic strategies.

This comprehensive systematic review and meta-analysis, published in The Lancet Public Health, evaluates the relationship between daily step count and a wide range of adult health outcomes. Unlike previous reviews that mostly focused on all-cause mortality and cardiovascular disease, this study incorporates data from 57 studies across 35 cohorts to examine broader health outcomes such as cancer, type 2 diabetes, dementia, depressive symptoms, physical function, and falls. Data from 24 cohorts were used in meta-analyses.

This study, using data from the EuroTR registry, investigated the impact of prior heart failure hospitalizations (HFHs) on outcomes in patients undergoing tricuspid transcatheter edge-to-edge repair (T-TEER) for symptomatic tricuspid regurgitation (TR). Among 1000 patients analyzed, 63.9% experienced at least one HFH in the year before T-TEER. These patients presented with more advanced heart failure symptoms, worse renal function, and higher natriuretic peptide levels. Despite similar procedural success across all groups—defined as achieving residual TR grade ≤2—the presence of prior HFHs was linked to significantly higher risks of all-cause mortality and combined mortality/HFH outcomes.